|
 |
- Search
| Intest Res > Volume 19(4); 2021 > Article |
|
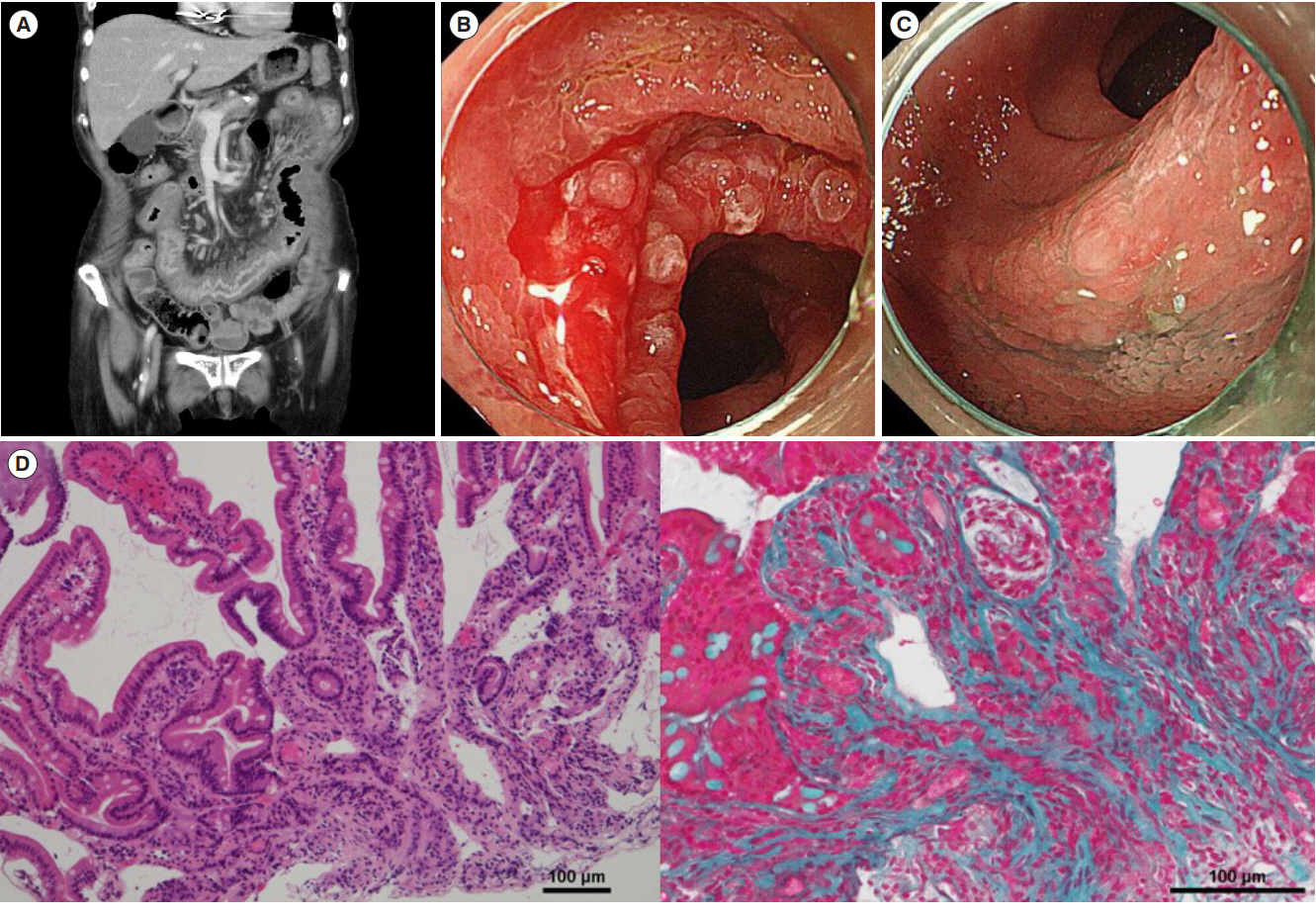
Question: An 80-year-old woman who was taking valsartan and amlodipine for hypertension, esomeprazole, apixaban and diltiazem for atrial fibrillation, and levothyroxine for chronic lymphocytic thyroiditis presented to our hospital with abdominal pain, vomiting and diarrhea. A blood test showed inflammation and malnutrition (white blood cell 4.9 × 103/μL, hemoglobin 11.5 g/dL, platelet 17.2 × 104/μL, total protein 5.5 g/dL, albumin 2.5 g/dL, aspartate aminotransferase 32 U/L, alanine aminotransferase 19 U/L, blood urea nitrogen 26.0 mg/dL, Cr 1.10 mg/dL, Na 134 mEq/L, K 3.9 mEq/L, and C-reactive protein 20.9 mg/dL). A stool culture showed commensal bacteria and a Clostridium difficile test was also negative. A computed tomography scan revealed severe inflammation of the small intestine, especially in the upper small intestine (Fig. A). We did single balloon enteroscopy and observed the duodenum and almost all of the upper small intestine. It showed erythema, mucosal fragility and villous atrophy enhancing mucosal fissures, and they looked like scalloped mucosa of celiac disease (Fig. B). Indigo carmine clearly revealed villous atrophy as shown in Fig. C. A pathological test of the small intestine showed collagen deposition and intraepithelial lymphocytosis (Fig. D: left, H&E; right, Elastica-Masson staining). At first, the patient was diagnosed with infectious enteritis and received conservative treatment with antibiotics (levofloxacin, ceftriaxone, tazobactam/piperacillin) for 3 weeks; however, the symptoms did not improve. Then, we did blood test again and it revealed negative for anti-transglutaminase and anti-endomysial antibodies. Therefore, we diagnosed her with a different enteritis, and began treating her with steroid therapy (prednisolone 30 mg/day). She improved slightly; however, she got worse during steroid tapering. Written informed consent was obtained. What is the diagnosis?
We eventually diagnosed the patient with valsartan-associated sprue-like enteropathy (VSE). She was taken off valsartan and began to improve. She was discharged from our hospital 19 days after valsartan discontinuation. Upon follow-up, she has not relapsed for 1 year. Her histocompatibility antigen (HLA) was HLA-DQ5/9.
Rubio-Tapia et al. [1] reported about olmesartan induced spruelike enteropathy in 2012. It is thought that the pathogenesis involves olmesartan strongly blocking angiotensin II receptor type 1 on intestinal epithelial cells, which causes apoptosis of enterocytes and disorder of intestinal immune homeostasis [1,2]. The enteropathy induces diarrhea, weight loss, vomiting, and abdominal pain among other symptoms. A negative blood test result for anti-transglutaminase or anti-endomysial antibodies and a positive result for villous atrophy, collagen deposition and intraepithelial lymphocytosis are helpful for a correct diagnosis. Rubio-Tapia et al. also reported that 81% of the patients in their study had HLA-DQ2 or HLA-DQ8. The patients received a gluten-free diet, steroid therapy, antibiotics and pancreatic enzymes for treatment [1]; however, the discontinuation of the drug was effective for all of the patients [2].
Lately, studies have suggested that some angiotensin 2 receptor blockers (ARBs) have induced enteropathy [3]. The ratio of patients with VSE was 1.2% in patients with ARB-associated sprue-like enteropathy [3]. To the best of our knowledge, there are only a few articles about VSE [4,5]. Those cases, including our case, sometimes cause severe enteritis. Therefore, it is necessary to pay attention to this disease in cases with enteritis.
Our case did not improve with steroid therapy, and therefore discontinuation of the ARBs seemed to be the best treatment for the enteropathy. Also, our case exhibited severe enteritis and atypical HLA. When we see enteropathy in atypical cases, it is important to try discontinuing ARBs as a treatment option.
ADDITIONAL INFORMATION
REFERENCES
1. Rubio-Tapia A, Herman ML, Ludvigsson JF, et al. Severe spruelike enteropathy associated with olmesartan. Mayo Clin Proc 2012;87:732-738.



2. Ianiro G, Bibbò S, Montalto M, Ricci R, Gasbarrini A, Cammarota G. Systematic review: sprue-like enteropathy associated with olmesartan. Aliment Pharmacol Ther 2014;40:16-23.


3. Kamal A, Fain C, Park A, et al. Angiotensin II receptor blockers and gastrointestinal adverse events of resembling spruelike enteropathy: a systematic review. Gastroenterol Rep (Oxf) 2019;7:162-167.