Landscape of inflammatory bowel disease in Singapore
Article information
Abstract
Inflammatory bowel disease (IBD), primarily Crohn’s disease and ulcerative colitis, had been widely recognized to affect the Western population. However, the notable rise in prevalence of IBD in Asia, including Singapore, had garnered much attention to the causal role of the shift in trend, and more importantly, effective and safe management of the conditions of these groups of patients in terms of therapy, healthcare economics as well as patient well-being. This review presents a summary of the current landscape of IBD in Singapore, and discuss on areas that can be explored to improve and better understand the local condition, as prevalence continues to grow.
INTRODUCTION
Inflammatory bowel disease (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), is a debilitating lifelong condition with significant health and economic costs with a prevalence rate in Western countries at 29.3 per 100,000 and 24.3 per 100,000 persons respectively [1,2]. Recently, several groups leveraged on existing global epidemiology data available to perform various statistical analysis modelling to predict future prevalence and IBD disease burden in Asia, Europe and North America, with an aim to inform healthcare policy makers on the prevalence trends, and to better prepare the healthcare systems. Through these statistical modelling, it was predicted that in year 2030, Canada and Portugal would expect up to 981 and 325 IBD cases per 100,000 individuals respectively [3,4], whereas a further increase in prevalence is also forecasted in Asian countries such as Iran (2.5-fold), India (4-fold), Southeast Asia (1.6-fold) by 2023 [5].
Interestingly, epidemiological studies also revealed that children of parents that had migrated from region with low IBD prevalence in Asia, and currently residing in developed countries, exhibit similar high incidence of IBD compared to offspring of non-immigrants, suggesting how disease risk could be more influence by earlier life exposure to environmental antigens [6].
Over the past two decades, while IBD case in Asia, including Singapore, has risen significantly, it is still considered relatively lower compared to Western countries, and therefore sometimes misdiagnosed as gastrointestinal tuberculosis or irritable bowel syndrome leading to delay in treatment. The Asia-Pacific Crohn’s and Colitis Epidemiology Study is a collaboration project between 11 countries across Asia and Australia, focusing on research of IBD in Asia-Pacific, and they have reported an incidence of IBD in Asia to be 0.5–3 per 100,000 individuals, in which early course disease progression was comparable between the East and West [7-9]. The same study also reported that few patients with early-stage UC undergo surgery in Asia, where as CD patients frequently progress to complicated disease and have accelerated use of immunosuppressants. Asian IBD patients might also exhibit slightly different clinical phenotype, as compared to Western patients, including increased ileocecal involvement in CD, reduced familial aggregation, less extraintestinal manifestations and worse clinical outcomes for older-onset patients with UC [10].
Recently, Kaplan and Windsor [11] showed that the evolution of IBD can be classified into 4 epidemiological stages using actual data obtained from different regions around the world. Developing countries are in the Emergence stage, newly industrialized countries are in the Acceleration in Incidence stage, and Western European regions are in the Compounding Prevalence stage. The Western European region is in the Compounding Prevalence stage, after which there may be an increase in mortality due to coronavirus disease 2019 (COVID-19) infections, suggesting that the region will eventually move into a Prevalence Equilibrium stage. Different genetic makeup and environmental exposures in different regions are likely the reason for this difference and therefore, careful evaluation of the differences and rates in epidemiologic trends may help researchers and clinicians estimate disease burden and understand the reasons behind these differences, which may hold the key to unravel the etiology of Asian IBD.
IBD PREVALENCE IN SINGAPORE
Singapore is an ethnically heterogeneous city-state with a population made up of Chinese (77%), Indians (7.5%), and Malays (14%). Currently, it is estimated that there are 1,500 individuals who may be suffering from IBD in Singapore (incidence rate of 1.06 per 100,000 person), of which 200 are children [12]. The Singapore General Hospital saw close to 600 patients diagnosed with the disease in the year 2017 a 2-fold increase from a decade ago in 2007 [13]. The National University Hospital in Singapore saw a striking 8-fold increase in IBD patients, from below 50 in 2013 to close to 400 cases in 2018 [13]. Nevertheless, according to a recent systematic analysis for the Global Burden of Disease Study involving 195 countries and territories between 1990 and 2017, Singapore had the lowest age-standardized death rate (0.08 per 100,000 population) [14].
Like adult IBD, incidence of pediatric IBD, although relatively uncommon in Singapore, has also dramatically increased over recent decades, with an incidence of 1.26 per 100,000 according to a recent Singapore cohort study conducted during the period of 1994 to 2015 [15]. More concerning is that the younger age disease onset, and higher proportions of perianal and stricturing/penetrating diseases required, suggested a more aggressive disease characteristics than those reported in the West. In this study the authors also concluded that Indians had a disproportionately high representation, while positive family history was rare (1.3%). Earlier onset in pediatric IBD in Singapore and more florid presentation may suggest different genetic and environmental influences specific to Asian children [16]. One potential attribution towards early onset of IBD, especially severe IBD in the first month of life, is mutations within the interleukin-10 (IL-10) receptor RA and/or RB that mediates suppression of the immune system [17]. More studies will be required to demonstrate whether Asian, as well as Singapore, early onset patients also reflect disruption within the IL-10 receptor signaling pathway and if so, one potential treatment would be stem cell transplantation which had been demonstrated to be effective in several Western patients [17,18].
In a separate study on Singapore and Malaysia IBD cohorts, 83% of the children with IBD had reported use of complementary and alternative medication (CAM), including probiotics, vitamins/minerals (e.g., vitamin D, multivitamins, vitamin C, iron), food-based therapies (e.g., fish oil, aloe vera, barley, turmeric, green tea, etc.), traditional medicines (e.g., traditional Chinese medicine/traditional Indian and Malay medicine) and/or mind/body practices (e.g., Chinese qi gong) [19]. There was a weak negative association between the use of CAM and self-rated disease activity reported (r=−0.257, P=0.041), but patients with more severe disease activities are less likely to use CAM as compared to patients with milder phenotype. The most common source of CAM knowledge was from friends and family (45%), followed by the internet (35%), books (10%), magazines or newspapers (5%), and medical staff (5%). Specifically, food-based CAM therapies was the only CAM category in which users reported significant self-perceived efficacy, with 67% agreeing that there were improvements in symptoms following CAM use (P=0.009). It is important to identify patients who are using CAM as these are groups that are likely to drop out of conventional therapies, and that the CAM might have adverse side effects as well. Separately, there had been also emerging evidence and supporting guidelines in Asia supporting the use of exclusive enteral nutrition over corticosteroids as first-line induction therapy for its superior outcomes in mucosal healing and growth [20]. A particular study involving Singaporean cohort similarly demonstrated a 91% remission rate in 40 newly diagnosed pediatric CD patients with 8 weeks of exclusive enteral nutrition, with early initiation of azathioprine maintenance therapy within 1 month of diagnosis sustaining a remission rate of 80% and 73% at 6- and 12-month post-induction, respectively [21].
HEALTHCARE ECONOMICS OF IBD IN SINGAPORE
Public health insurance coverage rate is relatively high in Singapore, which is also as seen in other Asian countries such as Taiwan, Korea, China, and Japan [22]. However, while most common tool for diagnosing IBD including colonoscopy is mostly free or highly covered by insurance in these countries, IBD patients in Singapore is expected to pay for such services, with insurance co-payment between 10% and 90% [22]. IBD patients are also expected to pay for conventional therapies and at a higher cost when compared to countries like India, as well as for biological products at the range of US $15,000 to US $25,000 per patient per year [22]. Fecal calprotectin test is available in clinical practice in Singapore, costing about US $40 to US $80 [22].
Biological products including infliximab, adalimumab, and golimumab are treatment currently listed on the Medication Assistance Fund under the Singapore Ministry of Health. However, vedolizumab, a monoclonal antibody that specifically binds to α4β7 integrin in the gut to reduce chronic intestinal inflammation, is not included given the cost-effectiveness and alternative treatments options available there were already included in the Medication Assistance Fund [23]. Despite this, increasing recent real-world evidence data and clinical trials (e.g., GEMINI registrational trials) continue to support vedolizumab as an effective treatment alongside with other first-line agent for the induction and maintenance of remission in IBD [24]. Vedolizumab received regulatory approval from the Health Science Authority in Singapore in February 2016 for the treatment of IBD.
In addition, other new IBD treatment includes ustekinumab (a monoclonal antibody targeting IL-12 and IL-23) that had obtained the Health Science Authority regulatory approval in February 2018 for the treatment of moderate to severely active CD adult patients that had failed or intolerant to immunomodulators or corticosteroids. In 2020, a study trial involving 22 Singapore-Asia cohort demonstrated that the safety and efficacy of ustekinumab were comparable to Western data [25]. Even more recently, tofacitinib (Janus kinase inhibitor) was also granted local regulatory approval in 2021 for moderate to active UC patients that had inadequate/lost response or intolerant to either conventional therapy or a biologic agent.
In a separate cohort study conducted in 2016 involving 490 IBD patients that were screened by the Singapore General Hospital indicated that patients with suboptimal controlled disease, infections, and on biological products had higher healthcare utilization [26]. CD patients required biological products and steroid treatment spent more on medications. Further studies measuring cost saving of biological products and immunomodulators to achieve remission will assist in treatment decision for Asian IBD patients.
NATIONAL IBD REGISTRY
Singapore currently does not have national registry for adult IBD unlike in many other countries such as the UK and Denmark, where data will be collected and made available [27,28]. Having a national registry for IBD will be particularly useful to ensure that therapies and clinical management of IBD patients are in accordance with the national clinical guidelines, as well as for audit purposes. In addition, the database can provide valuable resource and platform for a wide range of research in IBD, including basic science, translational research, and clinical/epidemiological studies.
Interestingly, there is currently ongoing efforts to establish an Asian Registry on Childhood Inflammatory Bowel Disease at the Singapore Clinical Research Institute, which is a national academic research organization dedicated to enhance the standards of human clinical research. The registry will collect and store data on clinical presentation, diagnostic workup, endoscopic evaluation and histology and management of children with IBD at the National University Hospital and collaborative study sites (local and regional). The main goal of this registry is to identify disease patterns amongst the Asian pediatric IBD cohort, and to pool valuable clinical data that would be of scientific interest to the global community managing IBD. It also envisioned to leverage on the registry to allow accurate analysis of specific patient subgroups, e.g., very early-onset CD, which would be of rare incidence in individual centers. In addition, having a common registry platform would also enable individual medical centers to standardize how the clinical course of pediatrics IBD is characterized, and enable a meaningful comparison between regional and global pediatric IBD data. Finally, the data collected from the registry would allow individual clinicians and hospitals across Asia to monitor short-term and long-term patient outcomes, adverse events after treatment, thus improving management strategies and allowing for better healthcare services to be designed for pediatric IBD.
HEALTH-RELATED QUALITY OF LIFE OF IBD PATIENTS IN SINGAPORE
It is widely accepted that the health-related quality of life (HRQOL) of IBD patients is significantly affected and has increasingly becoming an important aspect of medical decision-making, as improving HRQOL is a major goal of therapy and value-based healthcare. The Singapore General Hospital IBD center recently conducted an analysis of local IBD patient’s HRQOL using short IBD questionnaire (SIBDQ), Short Form-36 physical and mental component summary (SF-36 PCS/MCS) and EuroQol 5-dimensions 3-levels (EQ-5D-3L) and visual analogue scale (VAS). They found that presence of active disease, use of corticosteroids, presence of extraintestinal manifestation and unemployment were the few key factors that affect the HRQOL [29]. There was no difference reported between the HRQOL of UC and CD patients [29].
IBD PATIENT SUPPORT
From diagnosis to management, IBD can cause psychosocial challenges to patients and their caregivers. Therefore, patient support groups (PSGs), such as the Crohn’s and Colitis Society of Singapore registered under the Ministry of Health in Singapore, can play a significant role in managing the non-therapeutic aspects to support patients during their life journey with IBD [12].
As IBD is relatively rare in Asia and unfamiliar to most people, PSGs can help promote local public awareness of the disease, and through organized activities, provide IBD patients a platform for networking and interaction with other IBD patients and share experiences. PSGs can also act as an advocate for IBD patients through active engagements with relevant agencies to launch initiatives for the benefit of local IBD patients. For example, Singapore IBD PSGs launched the “Can’t Wait” card in 2014 to allow IBD patients get priority access to public toilets, while side-stepping embarrassing explanations, as well as giving confidence to patients to step out of isolation at home.
PSGs in Singapore can act as a central point-of-contact to facilitate IBD research and development, to bring different groups including scientist, clinicians, government and industries together for better synergies in understanding problem statements and providing technological solutions. This can help accelerate Asia/Singapore research and development effort to better understand Asian IBD and add on existing information based on Western context, including local genetic makeup, potential long-term complications (e.g., risk of colitis-associated cancer). This will have significant impact on therapy and disease management plans for IBD patients.
CONCLUSION
While prevalence of IBD in Asia is still lower than in the West, it is certainly on the rise and can be as severe or more severe in Asia than in the West [30]. The emergence of IBD in Asia will result in the need for specific health care resources, and offers a unique opportunity to study etiologic factors. Given the uniqueness of the Asian phenotype, as well as Singapore push and support on the National Precision Medicine, IBD research in Singapore can not only unveil interesting biology in the pathogenesis of IBD, but more importantly benefitting patients in managing their IBD conditions (Fig. 1).
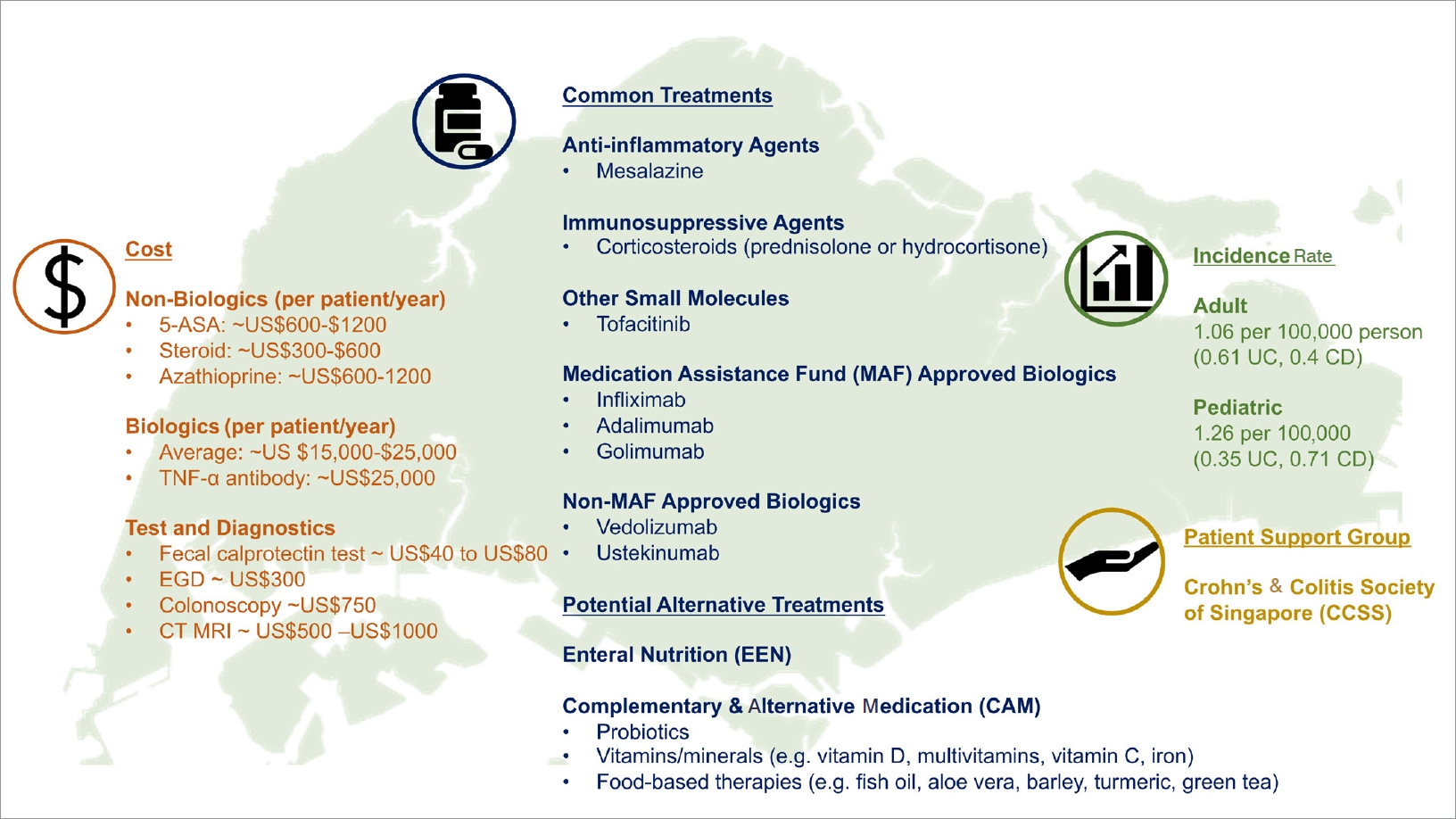
Overview of the inflammatory bowel disease (IBD) landscape in Singapore. The uniqueness of IBD in the aspect of incidence rate, cost, common treatments and IBD patients support group has been summarized. 5-ASA, 5-aminosalicylic acid; TNF-α, tumor necrosis factor α; EGD, esophagogastroduodenoscopy; CT, computed tomography; MRI, magnetic resonance imaging; UC, ulcerative colitis; CD, Crohn’s disease; US, United States.
Notes
Funding Source
This work has been supported by grants from the Ishibashi Foundation for the Promotion of Science, Japan Society for the Women Health Science, Fukuoka Clinical Medical Research Award and the Japanese Society for the Promotion of Science (Nos. 18K07987 and 21K07996) to Mizoguchi E.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Data Availability Statement
Not applicable.
Author Contribution
Conceptualization: Low D, Swarup N, Okada T, Mizoguchi E. Data curation: Low D, Mizoguchi E. Formal analysis: Low D. Funding acquisition: Mizoguchi E. Investigation: Low D, Swarup N, Okada T, Mizoguchi E. Project administration: Low D, Swarup N. Resources: Low D, Swarup N. Supervision: Low D, Swarup N, Mizoguchi E. Validation: Swarup N, Okada T. Visualization: Low D, Mizoguchi E. Writing - original draft: Low D, Swarup N, Okada T, Mizoguchi E. Writing - review & editing: Low D, Swarup N, Okada T, Mizoguchi E. Approval of final manuscript: all authors.
