Vedolizumab does not increase perioperative surgical complications in patients with inflammatory bowel disease, cohort study
Article information
Abstract
Background/Aims
Biologics are increasingly used to manage ulcerative colitis (UC) and Crohn’s disease (CD). However, even with earlier usage of biologic therapy, a significant proportion of patients will require surgery. Vedolizumab is an anti-integrin antibody that is increasingly used given that it is more gut selective and associated with fewer side effects. The aim of this study is to assess the effect of vedolizumab compared to anti-tumor necrosis factor (anti-TNF) therapy on the perioperative complications in patients undergoing surgery for inflammatory bowel disease (IBD).
Methods
Retrospective review of patients treated for IBD at a tertiary care center between 2013 and 2017. Rates of 30- and 90-day complications for patients on vedolizumab were compared to patients on anti-TNF regimens.
Results
One hundred and ninety-nine patients met inclusion criteria with 87 (43%) patients undergoing surgery for CD, 111 (55.8%) for UC and 1 (0.5%) for indeterminate colitis. Thirty-eight patients received preoperative vedolizumab and 94 received anti-TNF. There were more males and lower body mass index in the anti-TNF group. There was no significant difference in overall rate of complications at 30 or 90 days. There was a trend for lower leak rate vedolizumab group (0% for vedolizumab vs. 2.1% for anti-TNF at 30 days, P = 1.00; 0% for vedolizumab vs. 1.1% for anti-TNF at 90 days, P = 1.00). Multivariate analysis showed low albumin (< 3.6 g/dL) at the time of surgery to be a significant risk factor for overall and infectious complications at 90 days (odds ratio, 3.24; 95% confidence interval, 1.12–8.79; P = 0.021).
Conclusions
Perioperative vedolizumab does not increase rates of perioperative complications in IBD surgery when compared to anti-TNF medications.
INTRODUCTION
Inflammatory bowel disease (IBD) rates are continuing to grow in the United States and worldwide [1]. Introduction of biologics has offered a hope that with improved disease control rates of surgical interventions for disease management will be reduced [2-4]. However, after an initial decrease [5-8], rates of surgery have plateaued for both ulcerative colitis (UC) and Crohn’s disease (CD) while significant concerns have been raised about increasing rates of peri-operative complications [2-4]. Anti-tumor necrosis factor (anti-TNF) medications, in particular infliximab, have been shown to increase rates or perioperative infectious complications although this data remains controversial [3,8-10]. It has also been suggested that concerns about anti-TNF related surgical complications is at least in part responsible for the increased rate of 3 stage surgery for UC in the United States [10].
Vedolizumab is an α4β7 anti-integrin antibody that has been increasingly used in both UC and CD. The α4β7 inhibition is specific to the gut, however, concerns remain about overall effects on perioperative surgical complications [11-13]. Initial report by Lightner et al. [9] indicated increase in rates of perioperative infectious complications. In contrast though, Yamada et al. [14] did not confirm these concerns in their cohort undergoing surgery after exposure to vedolizumab.
Given the discrepant data on the perioperative surgical risk, we sought to investigate effects of vedolizumab compared to anti-TNF medication’s effect on perioperative complications in patients undergoing surgery for UC and CD at a tertiary care referral center for IBD.
METHODS
The study was performed at a tertiary care academic medical center with a center for IBD and colorectal surgical service. The study population was identified through a single center institutional database collected using ICD-9 (555.x and 556.x) and ICD-10 codes (K50.x and K51.x) for UC and CD. Data were collected retrospectively from March 2013 to August 2017. All charts were manually reviewed to confirm the diagnosis and for data extraction. Inclusion criteria were adults with IBD on vedolizumab or anti-TNF agents who received their last dose within 4 weeks of surgery. Electronic medical records were reviewed for patient information on demographics, IBD history, perioperative details of age, gender, preoperative diagnosis, body mass index (BMI), C-reactive protein, segment removed, urgency of surgery, indication for surgery, extent of disease, disease severity, previous IBD medication used, vedolizumab or anti-TNF medications within 4 weeks of surgery, preoperative corticosteroid use and Charlson comorbidity index (CCI) score.
The primary endpoint was postoperative complications at 30 and 90 days in patients treated with vedolizumab compared to anti-TNF medications. Complications were defined as any of the following conditions: urinary retention, surgical site infection, ileus, deep vein thrombosis, pulmonary embolism, small bowel obstruction, postoperative bleeding, intra-abdominal abscess, leak, return to operating room, dehydration, readmission, Clostridium difficile infection and other complications.
Continuous variables were expressed as mean (standard deviation) or median (interquartile range), normality was checked with the Shapiro-Wilk test. Differences between continuous variables where assessed with t-test and Wilcoxon rank-sum test where indicated. Fisher exact test and chi-square were used to compare categorical variables. Stepwise multivariate logistic regression analysis was used to evaluate the effect of the drug by adjusting for potential confounders, selected based on univariate association with the outcome or drug indicator.
The study was approved by the Institutional Review Board of Beth Israel Deaconess Medical Center (protocol number: 2010-P-000263/1). The informed consent was waived. This study was registered with Research Registry and has been reported in line with STROCSS criteria [15].
RESULTS
1. Patients Characteristics and Surgical Demographics
During study period 199 patients were eligible for analysis. Eighty-seven patients (43%) underwent surgery for CD, patients (55.8%) underwent surgery for UC and 1 patient with indeterminate colitis. The most common procedures performed were total proctocolectomies in 68 patients (34.3%), followed by 50 (25.3%) right hemicolectomies, 32 (16.2%) subtotal colectomies, 27 (13.7%) proctectomies, 9 (4.6%) left hemicolectomies, and 4 (2%) ileostomies. The rest of the procedures constitute entero-cutaneous fistula takedowns, small bowel resections, lysis of adhesions and colostomy creation. There were 38 patients in vedolizumab group and 94 patients in anti-TNF group. The anti-TNF group was comprised of 53 (57%) patients with infliximab, 37 (40%) adalimumab, 2 (2%) golimumab and the remaining with certolizumab. There were more males (60% vs. 34%, P = 0.007) and lower BMI (22.7 vs. 26.8, P = 0.016) in the anti-TNF group when compared to vedolizumab group. Otherwise there were no other significant differences in preoperative characteristics, comorbidities or surgeries performed (Table 1).
Stoma formation rates were also similar between groups with overall rates (for both UC and CD) 26 (75.3%) in vedolizumab group compared to 59 (74.7%) in anti-TNF group (P = 0.964) and included planned stomas (e.g., patients undergoing ileal pouch-anal anastomosis surgery). Subgroup analysis looking at CD also showed higher, but not statistically significant rates of stoma formation in vedolizumab group (50%) when compared to anti-TNF group (31%) (P = 0.336).
2. Postoperative Complications
Rates of postoperative complications at 30 and 90 days were also similar between the groups in urinary retention (P = 1.00 at 30 days, P = 1.00 at 90 days), ileus (P = 0.11 at 30 days, P = 0.15 at 90 days), bowel obstruction (P = 0.15 at 30 days, P = 0.42 at 90 days), acute renal failure (P = 0.29 at 30 days, P = 0.63 at 90 days), thromboembolic events (P = 1.00 at 30 days, P = 0.72 at 90 days) and anemia requiring blood transfusion (P = 0.59 at 30 days, P = 0.40 at 90 days) (Table 2). Nevertheless, there was a noticeable higher rate of intra-abdominal abscess, but not statistically significant in anti-TNF group (12.8% at 30 days, 8.5% at 90 days) when compared to vedolizumab group (2.6% at 30 days, 0% at 90 days) (P = 0.06) (Table 2). Overall, the rates of ileus, acute renal failure, thromboembolic, C. difficile infection, urinary as well as need for blood transfusions were the same in both groups. There was no statistical difference in 90-day outcomes in subgroup analysis between infliximab and adalimumab (P = 0.68). Additionally, there was a higher rate of non-infectious complication, for UC compared to CD, 62% (n = 69) versus 46% (n = 40) (P = 0.02), respectively. With a similar trend of higher infectious complications (UC of 39.6% [n = 44] vs. CD of 27.6% [n = 24], P = 0.08), however, these not reaching statistical significance.
3. Risk Factors for Postoperative Complications
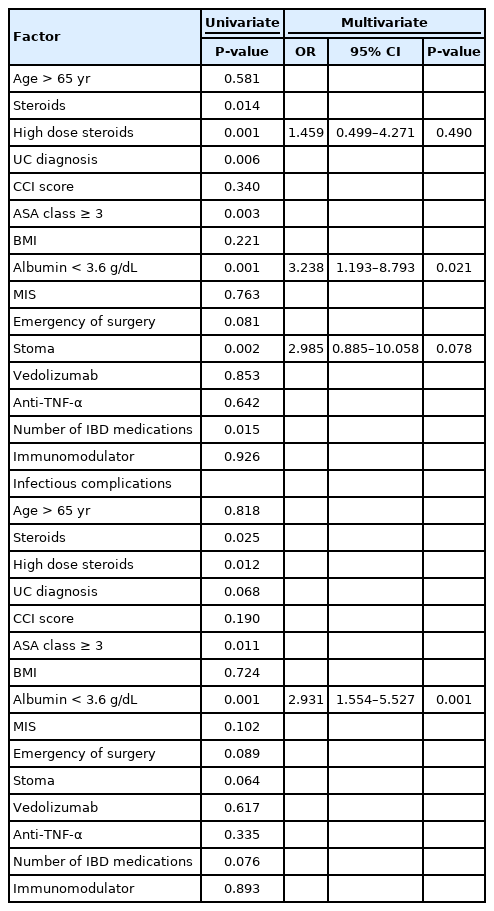
When assessing risk factors for complications in univariate analysis, use of steroids, high dose steroids (more than 20 mg prednisone equivalent per day), diagnosis of UC, American Society of Anesthesia class ≥ 3, low albumin levels, stoma formation and number of IBD medication at the time of surgery where statistically significant as risk factors for 90-day overall complications (Table 3). On the stepwise multivariate logistic regression model with the aforementioned variables, low albumin (< 3.6 g/dL; odds ratio [OR], 3.238; 95% confidence interval [CI], 1.193–8.793; P = 0.021) resulted as the only statistically significant factor with increased probability for overall complications (Table 3) at 90 days after surgery. Use of steroids at the time of surgery was also a significant risk factor for complications at 30 days (OR, 3.262; 95% CI, 1.157–9.198; P = 0.025). On the other hand, age (> 65 years), CCI score, BMI, minimally invasive surgery, immunomodulators (cyclosporine, thiopurines, and methotrexate) and urgency of surgery were not risk factors for postoperative complications.
DISCUSSION
In our study examining risk of postoperative complications, use of vedolizumab within 4 weeks of surgery did not increase risk of perioperative complications compared to anti-TNF medications and vedolizumab had a trend towards a lower rate of infectious complication.
Multiple medical options are currently available for treatment of IBD, including a number of biologics. However, despite recent advances, need for surgical intervention did not change significantly in this patient population and thus balance between using medical therapy to avoid surgery and avoiding complications if surgery is needed is very important in patients with IBD. Most, especially more recent medications, lack consistent data on their effect of perioperative complications. Lightner et al. [9] indicates that similar to anti-TNF medications, perioperative complications are increased with vedolizumab and especially with surgical site infection. In contrast, our data is more in line with findings by Yamada et al. [14] that the gut selective nature of vedolizumab is associated with lower rates of perioperative complications. Our data add to the current literature further supporting the safety of vedolizumab. Even with a large referral center for IBD with patients with severe disease, still no increase in drug related complications were seen. This is reassuring when compared to data with anti-TNF where current studies have suggested a possible increased risk of infectious complications. While the data does not provide guidance on which drug to choose when treating IBD, it should provide gastroenterologists and surgeons confidence that use of vedolizumab with severe IBD will not increase the risk of perioperative complications.
Rather than drugs increasing the risk, our data suggests there may be other predictors of complications. Similar to other reports, we found poor nutritional status (as reported by low albumin) and use of steroids to be significant risk factors for complications. Our study also suggests that a number of IBD medications at the time of surgery may be playing a significant role. The exact cause of this is unclear, but may be related to cumulative effect of these medications, each potentially suppressing different parts of immune response. It is also possible that this is a surrogate for overall sicker patient.
The strength of our study is that we examined both 30- and 90-day complications, accounting for delayed surgery related effects that may be missed by limiting analysis to only 30 days. In addition, we chose to limit our data set to patients who received medications within 4 weeks of surgery to include those patients with higher drug levels in them at the time of surgery. How long these medications last in the system and effect of low dose detectable levels on post-surgical outcomes is not well understood, but it has been suggested that even low dose can have negative effects on outcomes [16,17]. In our study, however, rates of complications with vedolizumab were still low in this potentially higher risk group of patients.
The main limitations of our study are its low numbers, especially in the vedolizumab group., even when combining both UC and CD patients. In addition, because of low numbers, it was not possible to generate purely non-biologic group (e.g., on mesalamine or nothing) for comparison without extending data further back, but that would then include patients not treated in the current standard of care with biologics and could skew the data. Limited data was available on dosing and intervals of anti-TNF medications used before surgery as well as levels and this was not included in the study. One of the important clinical outcomes, especially in patients with CD is a need for stoma, either planned (as assessed by preoperative risk) or unplanned (as decided in the operating room). Although we did not see the difference in rates of stoma formation in our study, because of limitations of this data set, being a retrospective study, it is not possible to determine what proportion of diversion in CD patients were planned or unplanned.
In conclusion, preoperative use of vedolizumab does not increase rates of postoperative complications and may have a better infectious complication profile when compared to antiTNF medications. Further prospective studies are needed to further evaluate effects of vedolizumab on surgery.
Notes
Funding Source
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contribution
Conceptualization: Poylin VY, Feuerstein JD. Data curation: Poylin VY, Cataneo J, Pastrana Del Valle J. Formal analysis: Poylin VY, Cataneo J, Pastrana Del Valle J. Investigation: Cataneo J, Pastrana Del Valle J. Methodology: all authors. Project administration: Poylin VY, Cataneo J, Pastrana Del Valle J. Supervision: Poylin VY, Feuerstein JD. Validation: Poylin VY, Cataneo J. Writing-original draft: Poylin VY, Cataneo J, Pastrana Del Valle J. Writing-review & editing: Poylin VY, Feuerstein JD. Approval of final manuscript: all authors.
Others
This work was conducted with support from Harvard Catalyst/The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102) and financial contributions from Harvard University and its affiliated academic health care centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, or the National Institutes of Health.
This article was presented at the Digestive Disease Week on June 2-5, 2018, in Washington DC, USA.