An oval-shaped calcification in Crohn’s disease patient with mechanical ileus
Article information
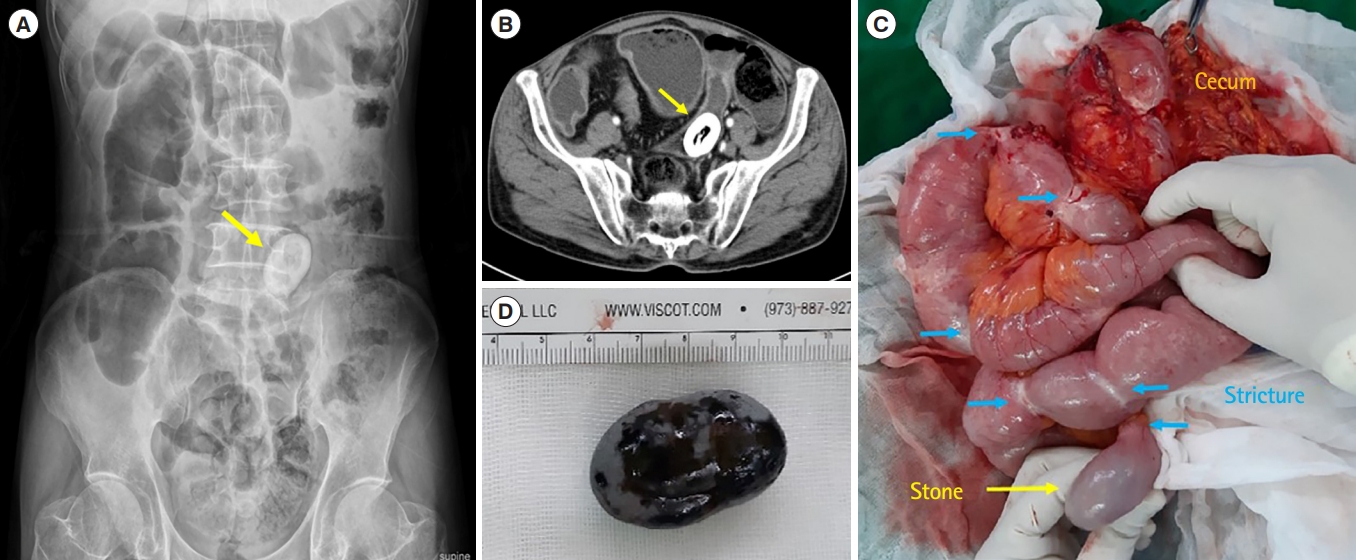
Question: A 65-year-old man presented with nausea and diffuse abdominal pain. The patient was very skinny with a height of 171.9 cm, weight of 52.1 kg, and body mass index of 17.6 kg/m2. He was diagnosed with Crohn’s disease 20 years previously. He had no history of surgery. On physical examination, the abdomen was distended without abdominal guarding. Laboratory findings were notable with hemoglobin 10.2 g/dL, total protein 5.49 g/dL, and albumin 3.27 g/dL. The inflammatory marker (C-reactive protein) was mildly elevated to 1.9 mg/dL. Serology for the human immunodeficiency virus was negative. Tumor markers, such as carcinoembryonic antigen, carbohydrate antigenic determinant, and α-fetoprotein, were within the normal range. On plain abdominal radiography, an oval-shaped, calcified, laminated white opaque on the left side of the sacrum was observed (Fig. A, arrow). Computed tomography showed mechanical obstruction of the small bowel with multiple short-segment strictures, and oval-shaped calcified mass in the ileum (Fig. B, arrow). After 4 days of fasting and conservative treatment, the patient’s intestinal obstruction improved, and stool pass and gas out were confirmed. Colonoscopy was performed, but endoscopic access to the small intestine was impossible due to stenosis of the ileocecal area. The study’s protocol was waived by the Institutional Review Board of Pusan National University Hospital. Written informed consent was obtained. Based on above information, what is the most likely diagnosis?
Answer to the Images: Mechanical Ileus Caused by Crohn’s Disease-Related Enterolith
The patient underwent laparotomy: the intraoperative findings revealed one irremovable stony palpable mass. Distally, there were multiple short segment strictures as well as a proximal small bowel dilatation from 390 to 470 cm below the Treitz ligament (Fig. C, yellow arrow indicating small intestinal enterolith and blue arrows indicating distal fibrotic stricture). Small bowel resection of approximately 60 cm including stricture around the enterolith and stricturoplasty were performed. The removed enterolith was identified as black ovals measuring 30 × 40 mm (Fig. D). Histopathological examination of the resected specimen confirmed the diagnosis of an acute and chronic inflammation and fibrosis for episode of Crohn’s disease without any sign of fistula, abscess formation and perforation, or malignant transformation.
Intestinal enteroliths are defined as endogenous foreign bodies in the gastrointestinal tract, and are a rare entity. The crucial pathogenetic factor in the development of intestinal enteroliths is stasis of the gastrointestinal tract, since a constant flow of the gastrointestinal contents usually does not form enteroliths [1]. Anatomic variations of the gastrointestinal tract (duplication cysts, diverticula) or pathologic conditions (strictures) can cause stasis and can form intestinal enteroliths. Crohn’s disease offers favorable conditions for the development of enteroliths because of its typical strictures that impair intestinal flow. Nevertheless, even in the largest literature review, Crohn’s disease-related intestinal enterolith are rare, including only 22 cases over a period of approximately 40 years [2]. Characteristically, Crohn’s disease-related enteroliths which are important clues to the presence of underlying stricture occurs only in patients with a long history of the disease and a long duration of symptoms. The duration of Crohn’s disease in previously published cases ranged from 7 to 40 years, with a median duration of 15.7 years [3]. The majority of Crohn’s disease-related enteroliths present with signs and symptoms of intestinal obstruction, and sometimes with perforation, bleeding or refractory anemia [4]. There is no evidence for prophylactic treatment of asymptomatic intestinal enteroliths in Crohn’s disease. The treatment of symptomatic intestinal enteroliths includes endoscopy (endoscopic dilatation for stenosis or endoscopy guided laser lithotripsy) or surgery (removal of the enteroliths and the management of the underlying stricture by either stricturoplasty and/or resection) [5]. Adenocarcinoma of the small intestine was found in a place where small intestine stones related to Crohn’s disease were surgically removed, so it is necessary to consider adenocarcinoma when Crohn’s disease and small intestinal enteroliths are accompanied, so meticulous inspection and biopsy of each proposed site of stricturoplasty are essential to rule out adenocarcinoma. In summary, Crohn’s disease-related enterolith occurs secondary to stricture formation with obstruction. The enterolith in patients with Crohn’s disease importantly indicates underlying stenotic disease. Although Crohn’s disease-associated small intestinal enterolith is rare, it should be considered in the differential diagnosis of mechanical ileus at Crohn’s disease, especially in patients with a long-standing history of Crohn’s disease and a long duration of symptoms.
Notes
Funding Source
This study was supported by the 2022 overseas training grant from Pusan National University Hospital.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Data Availability Statement
Not applicable.
Author Contribution
Conceptualization, data curation, formal analysis, methodology: Kwak YM, Baek DH. Project administration: Baek DH, Lee BC. Resources: all authors. Supervision: Baek DH, Lee BC. Visualization: all authors. Writing - original draft: Kwak YM. Writing - review & editing: all authors. Approval of final manuscript:all authors.