Perspectives of East Asian patients and physicians on complementary and alternative medicine use for inflammatory bowel disease: results of a cross-sectional, multinational study
Article information
Abstract
Background/Aims
Complementary and alternative medicine (CAM) is prevalent in East Asia. However, information on CAM in East Asian patients with inflammatory bowel disease (IBD) is scarce. We aimed to profile the prevalence and pattern of CAM use among East Asian IBD patients and to identify factors associated with CAM use. We also compared physicians’ perspectives on CAM.
Methods
Patients with IBD from China, Japan, and South Korea were invited to complete questionnaires on CAM use. Patient demographic and clinical data were collected. Logistic regression analysis was applied for predictors of CAM use. Physicians from each country were asked about their opinion on CAM services or products.
Results
Overall, 905 patients with IBD participated in this study (China 232, Japan 255, and South Korea 418). Approximately 8.6% of patients with IBD used CAM services for their disease, while 29.7% of patients sought at least 1 kind of CAM product. Current active disease and Chinese or South Korean nationality over Japanese were independent predictors of CAM use. Chinese doctors were more likely to consider CAM helpful for patients with IBD than were Japanese and South Korean doctors.
Conclusions
In 8.6% and 29.7% of East Asian patients with IBD used CAM services and products, respectively, which does not differ from the prevalence in their Western counterparts. There is a significant gap regarding CAM usage among different Asian countries, not only from the patients’ perspective but also from the physicians’ point of view.
INTRODUCTION
Inflammatory bowel disease (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), is a disabling and chronic relapsing inflammatory condition of the bowel. Without optimal treatment, it may cause irreversible bowel damage and lead to a negative impact on patients’ quality of life. Although IBD is the most prevalent disease in Western countries, the incidence of the disease has been rapidly increasing in East Asia, making it a global disease [1].
The cause of IBD is unknown, and there is no absolute cure. Although several therapeutic advances have been made in recent years, the unsatisfactory response rate, increased risk of relapse over time and adverse effects of therapy remain unmet clinical needs for the conventional management of IBD [2,3]. For instance, up to 40% of patients show primary or secondary nonresponse to biologic therapy targeting tumor necrosis factor (TNF), which has been regarded as the most effective treatment of IBD [4]. These limitations of current treatment may drive patients’ interest in complementary and alternative medicine (CAM).
CAM is defined as a group of diverse medical and health care systems, practices, and products that are not presently considered part of conventional medicine [5]. Patients with chronic diseases such as IBD seek CAM amid concerns of response failure or side effects of standard therapy [6,7]. The use of CAM by patients with IBD is remarkably high [8,9]. Meanwhile, doctors do not seem to be prepared to address CAM-related issues among their patients. A third of physicians are not comfortable discussing CAM with their IBD patients due to a lack of knowledge [10]. Medical care providers need to be aware of patients’ intentions to use CAM because CAM may have negative impacts on the care of IBD. First, it may negatively influence doctor-patient relationships, since CAM use reflects dissatisfaction with the current standard therapy [11]. Second, there might be a potential critical interaction between current therapy and CAM [12]. Third, CAM use is reported to be associated with poor compliance in patients [8].
With the substantial popularity and acceptance of CAM in the general population, the prevalence of CAM use differs by country because of various economic, social and cultural factors. CAM use is considered to be widespread in East Asia because traditional oriental medicine, which is one of the main streams of CAM, originated in this area [13]. In a systematic review exploring CAM use by the general population in 15 countries, the 12-month prevalence of CAM use varied widely from 9.8% to 76% [14]. Among these countries, the highest rates of CAM use were observed in East Asian countries, including Japan (76%), South Korea (75%), and Singapore (76%). However, the prevalence and pattern of CAM use in patients with IBD from these areas have not been fully evaluated or compared. In addition, IBD doctors’ perspectives on CAM are unknown in this area. We aimed to evaluate and compare the prevalence of CAM use in patients with IBD in China, Japan, and South Korea. Furthermore, we asked physicians for their opinions on CAM for patients with IBD.
METHODS
1. Study Design
This was a cross-sectional, multinational study conducted in China, Japan, and South Korea from November 2017 to March 2018. Patients diagnosed with IBD for at least 6 months in tertiary hospitals were eligible for the study. IBD diagnosis was made based on a detailed history, physical examination, and combination of endoscopic features, histology, radiographic findings, and laboratory investigations. Participants who were younger than 18 years old or who were not able to read questionnaires were excluded. On an outpatient basis, they were consecutively invited to complete a questionnaire on CAM use over the past 12 months. Patient demographic and clinical data were collected. Regarding physicians’ perspectives on CAM, we invited doctors to participate in the study using the network in the Clinical Research Committee of the Asian Organization for Crohn’s and Colitis. We asked them to report on whether CAM is beneficial or recommendable for their IBD patients. Questionnaires used in the study are provided as Supplementary Material. This study was approved by the institutional review board of all participating hospitals (IRB No. KNUH2017-09-007-004). Written informed consent was obtained.
2. Data Collection
Patient demographic data, such as age, comorbidities, and sex, were collected. comorbidities included hypertension, diabetes mellitus, renal disease, respiratory disease, atopy, and malignancy. Clinical data included disease duration, disease activity, current medication, previous IBD-related hospitalization, and surgery history. The disease activity of CD and UC was assessed by the Harvey-Bradshaw index (HBI) and the Simple Clinical Colitis Activity Index (SCCAI), respectively. Scores equal to or more than 5 reflected active disease on both the HBI and SCCAI [15,16]. For physicians, data on age, sex, practice type (such as primary or referral center), and specialty (including IBD specialist, general gastrointestinal physician, pediatrician, and surgeon) were collected.
3. CAM Assessment
CAM was categorized into services and products; services in the study included massage, acupuncture, naturopathic medicine, homoeopathy, relaxation, reflexology, aromatherapy, hypnosis, moxibustion or cupping, spiritual or religious healing, and chiropractic therapy, whereas products in the study included herbal remedies, ginseng, deer antler, Chinese medicine, St. John’s wort, chamomile, lavender, ginkgo biloba, kava kava, vitamins, probiotics, fish oils, and glucosamine [9]. At first, patients were asked whether they used CAM services or products in general during the last year. Then, if they used CAM, they were asked whether it was specifically related to IBD.
4. Statistical Analysis
The sample size was calculated on the assumption that there will be a 15% difference in the prevalence of CAM use between countries (60% vs. 45%). With a 20% withdrawal rate and 80% power to detect such a difference at a two-tailed significance level of 0.05, at least 220 patients from each country were required.
Differences in categorical data among groups were examined by using chi-square or Fisher exact test. For continuous variables among 3 countries, analysis of variance was used. The pairwise Wilcoxon rank-sum test was used for multiple measurements of the nonparametric data among groups. The prevalence of CAM was compared among countries with adjustment of confounders such as age, duration of disease, sex, comorbidities, disease activity, current medications and previous history of surgery and admission. Independent factors associated with CAM use were analyzed by logistic regression. Variables with P-values less than 0.05 were selected for multivariate analysis. Multiple comparisons were corrected using the Bonferroni method. All tests were two-sided, and a P-value < 0.05 indicated statistical significance. All statistical analyses were performed using R package version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
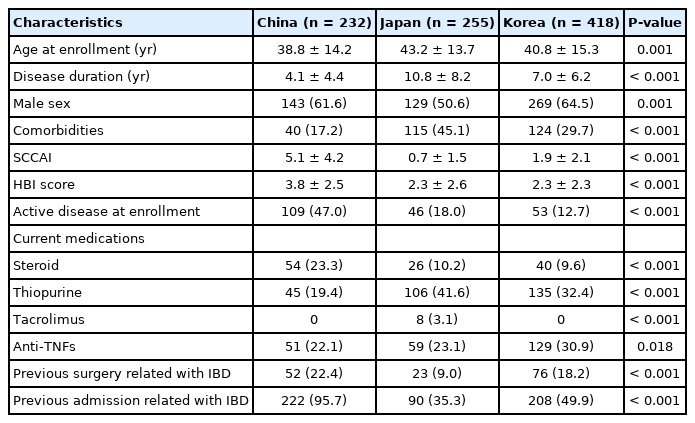
1. Baseline Characteristics of Patients
Fifteen institutions from 3 countries participated (China 5, Japan 3, and Korea 7), and 905 IBD patients were enrolled in the study (China 232, Japan 255, and South Korea 418). There was a significant difference in baseline characteristics among 3 countries (Table 1). Japanese patients were older (mean ± standard deviation [SD]: China 38.8 ± 14.2 years vs. Japan 43.2 ± 13.7 years vs. Korea 40.8 ± 15.3 years, P= 0.001) and had longer disease duration (mean ± SD: China 4.1 ± 4.4 years vs. Japan 10.8 ± 8.2 years vs. Korea 7.0 ± 6.2 years, P< 0.001) with higher rate of comorbidities (China 17.2% vs. Japan 45.1% vs. Korea 29.7%, P< 0.001) than patients from other countries. Chinese patients were more likely to have an active disease at enrollment (China 47.0% vs. Japan 18.0% vs. Korea 12.7%, P< 0.001) which was in line with higher rate of current steroid use (China 23.3% vs. Japan 10.2% vs. Korea 9.6%, P< 0.001) than patients from other countries. Tacrolimus was only used in Japanese patients with UC (3.1%, P< 0.001) while anti-TNF was more often used in South Korean patients (China 22.1% vs. Japan 23.1% vs. Korea 30.9%, P= 0.018). Previous surgery (China 22.4% vs. Japan 9.0% vs. Korea 18.2%, P< 0.001) and hospital admission related to IBD (China 95.7% vs. Japan 35.3% vs. Korea 49.9%, P< 0.001) were most observed in Chinese patients.
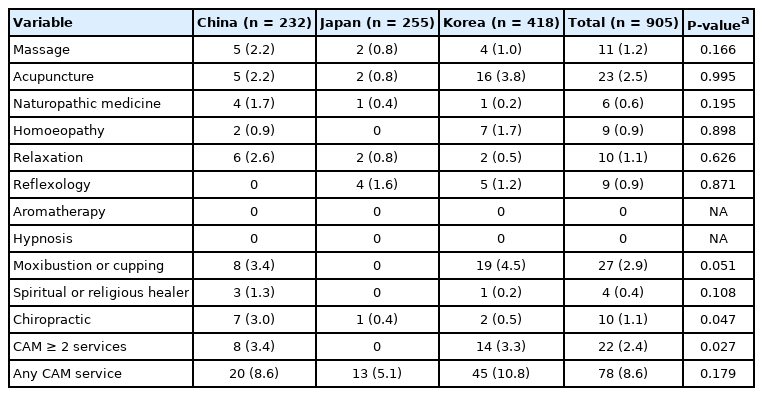
2. Prevalence of CAM Services and Product Use
Korean patients with IBD were generally more likely to use CAM services (P< 0.001) or products (P< 0.001) than were Chinese or Japanese patients (Supplementary Table 1). However, Chinese patients were more likely to use CAM products for the purpose of managing IBD (P< 0.001) (Supplementary Table 1). Up to 8.6% of patients with IBD consumed CAM services for the management of IBD during the last year, with no significant difference among nations (China 8.6% vs. Japan 5.1% vs. Korea 10.8%, P= 0.179) (Table 2). However, there was a significant difference in multiple service users ( ≥ 2 services) among nations (China 3.4% vs. Japan 0% vs. Korea 3.3%, P= 0.027). There was no difference in the use of each CAM service among patients with CD by country, except chiropractic service which was more utilized by Chinese patients (China 3% vs. Japan 0.4% vs. Korea 0.5%, P= 0.047). Among various CAM services, moxibustion/cupping was the most common service used by IBD patients (2.9%).
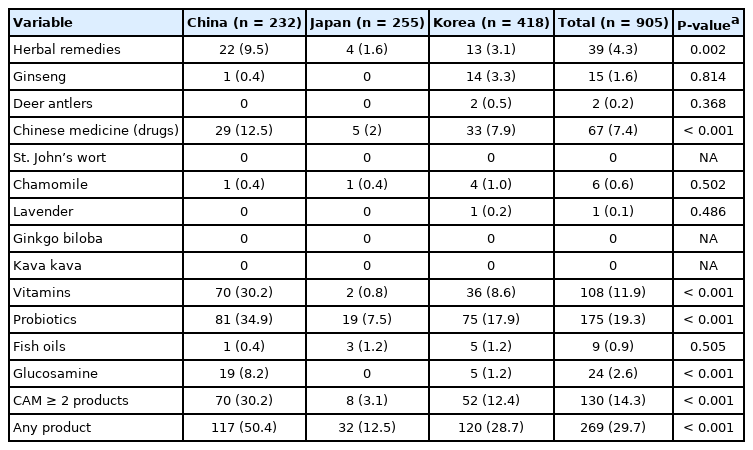
Prevalence of Complementary and Alternative Medical Services Usage in Inflammatory Bowel Disease Patients According to Countries
For CAM products, 29.7% of East Asian patients with IBD used at least 1 type of CAM product for the management of IBD during the last year with Chinese patients being the most common user (China 50.4% vs. Japan 12.5% vs. Korea 28.7%, P< 0.001). There was a significant difference in multiple product users ( ≥ 2 products) among nations (China 30.2% vs. Japan 3.1% vs. Korea 12.4%, P< 0.001). Chinese patients were more likely to use herbal remedies (P= 0.002), Chinese medicine (P< 0.001), vitamins (P< 0.001), probiotics (P< 0.001) and glucosamine (P< 0.001) than Japanese or Korean patients (Table 3). Probiotics was the most frequently used product (19.3%). Those comparisons of prevalence were conducted with the adjustment of age, duration of disease, sex, comorbidities, disease activity, current medications and previous history of surgery and admission related to IBD.
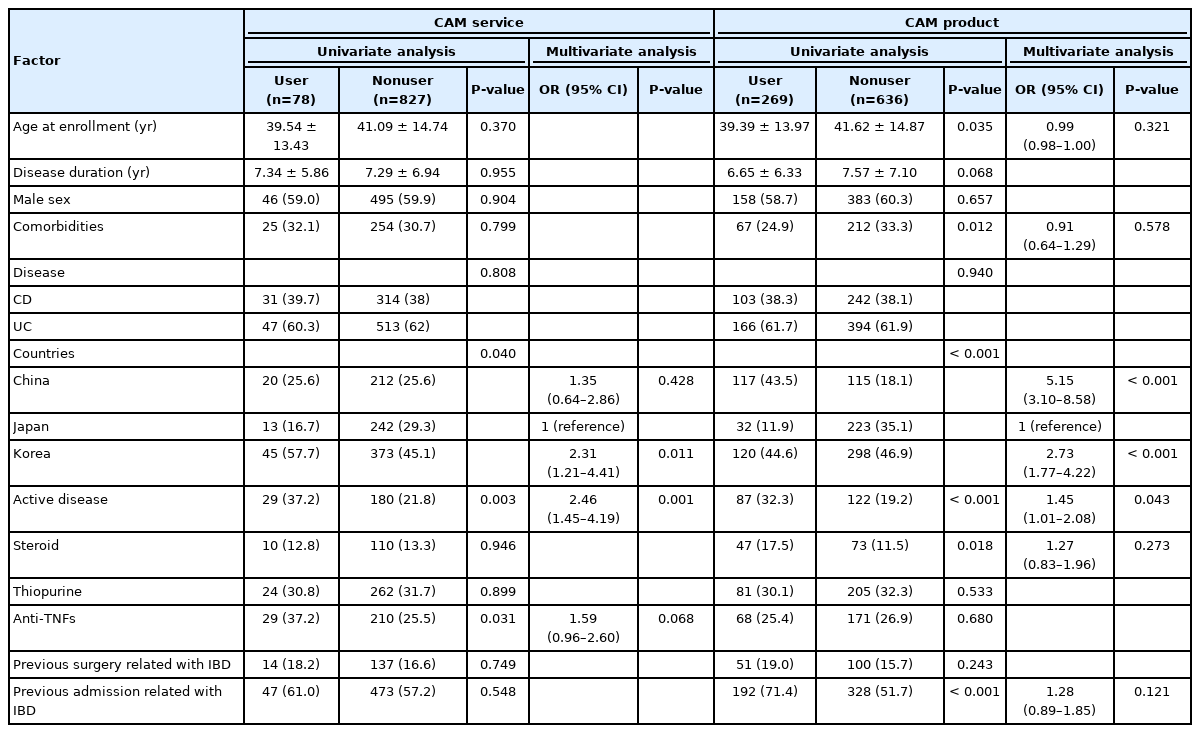
3. Predictive Factors of CAM Use
In univariate analysis, Chinese or Korean nationality (P= 0.04), active disease (P= 0.003), and anti-TNF use (P= 0.031) were significantly associated with CAM service use. Among them, multivariate analysis found South Korean nationality over Japanese (odds ratio [OR], 2.31; 95% confidence interval [CI], 1.21–4.41; P= 0.011) and active disease status (OR, 2.46; 95% CI, 1.45–4.19; P= 0.001) to be independent predictors of the use of CAM services. Younger age (P= 0.035), less comorbidities (P= 0.012), Chinese or Korean nationality (P< 0.001), active disease (P< 0.001), steroid use (P= 0.018) and previous admission related to IBD (P< 0.001) were significantly associated with CAM product use. Among them, Chinese (OR, 5.15; 95% CI, 3.1–8.58; P< 0.001) and South Korean nationality over Japanese (OR, 2.73; 95% CI, 1.77–4.22; P< 0.001) and active disease status (OR, 1.45; 95% CI, 1.01–2.08; P= 0.043) were found to be independent predictors of CAM product consumption in the multivariate analysis (Table 4).
4. Physicians’ Perception of CAM Usage for Their IBD Patients
Physicians were recruited for surveys from China (n = 20), Japan (n = 104), and South Korea (n = 29). The characteristics of these physicians are described in Supplementary Table 2. Chinese doctors were significantly younger (P= 0.003) and were predominantly female (P< 0.001) compared to doctors from other countries. More Japanese doctors worked at primary clinics than Chinese and South Korean doctors (P= 0.01). Therefore, these 3 factors (age, sex, and practice hospital) were adjusted in further comparisons among the 3 countries. Relaxation and probiotics were most frequently considered beneficial/recommendable services and products, respectively, by overall physicians. For CAM services, more Chinese physicians thought that acupuncture, naturopathic medicine, hypnosis, moxibustion/cupping, and spiritual healers were helpful, while more Japanese physicians regarded reflexology as an effective service for their IBD patients (Fig. 1A). For CAM products, Chinese doctors were more likely to consider herbal remedies, Chinese medicine, and glucosamine as beneficial/recommendable for their patients with IBD than were Japanese and South Korean doctors (Fig. 1B). Chinese and South Korean doctors regarded vitamins as helpful CAM for IBD compared with Japanese doctors (Fig. 1B).

The prevalence of complementary and alternative medicine service (A) and product (B) usage among patients with inflammatory bowel disease from 3 countries. The P-value is for the analysis of variance and was adjusted for physicians’ age and sex and the hospital type. aP<0.05, bP<0.01, cP<0.001.
Then, we tried to determine whether there was a difference regarding overall perceptions toward CAM among physician groups by measuring the median number of beneficial/recommendable forms of CAM considered by physicians from each country. Chinese doctors had a significantly higher median number (interquartile range) of beneficial/recommendable CAM services (China 2 [1–4] vs. Japan 1 [0–3] vs. Korea 1 [0–2]) or products (China 3 [3–5] vs. Japan 2 [1–3] vs. Korea 3 [2–3]) than did doctors from the other 2 countries, while there was no difference between Japanese and South Korean doctors (Fig. 2).
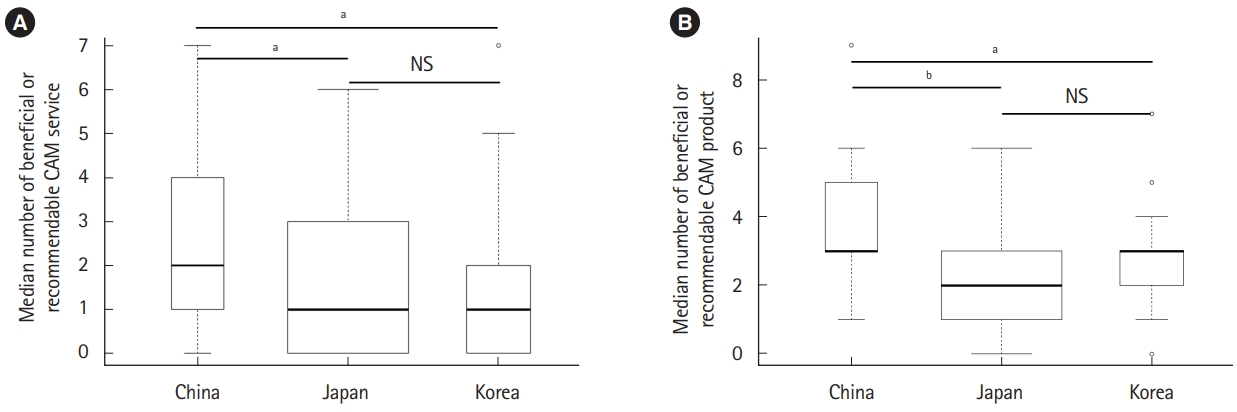
Comparison of physicians’ perspectives on complementary and alternative medicine (CAM) services (A) and products (B) for inflammatory bowel disease among 3 countries. The width of the box indicates the sample size of participants from each country. The P-value was calculated using the pairwise Wilcoxon rank-sum test after adjustment for physicians’ age and sex and the hospital type. aP<0.05, bP<0.001. NS, not significant.
DISCUSSION
This cross-sectional, multinational study demonstrated that approximately 1 in 10 and 1 in 3 East Asian patients with IBD used CAM services and products, respectively, for the management of IBD during the past year. Moxibustion/cupping was the most used CAM service by patients (2.9%) (Table 2), while most physicians considered relaxation to be a helpful CAM service for IBD (58%) (Fig. 1A). Probiotics were the most frequently consumed CAM products by patients (19.3%) (Table 3) and were also thought to be effective CAM products by most physicians (86%) (Fig. 1B). Chinese or South Korean patients over Japanese and current disease activity were independent predictors of CAM use for IBD management. In addition, Chinese doctors were more likely to perceive that CAM was helpful for IBD than were Japanese and Korean doctors (Fig. 2). To the best of our knowledge, this is the first report to compare the perspectives on CAM use among IBD patients from different East Asian countries as well as among physicians.
CAM use is highly prevalent among patients with IBD. In the studies reporting current or past CAM use together, the prevalence spanned a wide range (21%–77%) among patients with IBD [8,9,17-20]. Most studies in Western countries, such as North America and Northern Europe, exhibited a high prevalence of CAM use of 44% to 77% [8,9,18,21,22], which is higher than the prevalence in our study and in East Asian countries. Korean studies showed 28% to 38% prevalence in Korean IBD patients [23,24]. Chinese patients with IBD in Hong Kong also had a low prevalence of 33% compared with their Western counterparts [25]. However, caution should be taken when comparing the rate of usage among studies due to heterogeneous study designs and methodologies. For instance, there is a difference in the purpose of CAM use in patients with IBD. They may seek CAM for their IBD or for other health issues, including their general well-being. A survey-based study with 392 Canadian patients with IBD showed a prevalence rate of 62% for overall CAM usage, of which only one-third used CAM for IBD management similar with our result [8]. Another Western study [9,17] also reported that only 18% to 21% of IBD patients consumed CAM for their IBD, which is consistent with our results. In the present study, the prevalence of CAM service use was reduced to 8.6% for IBD management from 36.2% for overall indications, and the prevalence of CAM product use was reduced to 29.7% for IBD management from 60.2% for overall indications (Supplementary Table 1). As many patients use CAM for purposes other than IBD management, they may not report CAM use to their doctors. Therefore, this finding underscores the fact that doctors should actively engage in a discussion of CAM use with their IBD patients because CAM may cause a potential risk of drug interactions or liver toxicity [12,26,27].
We found a significant difference regarding perceptions of CAM use among patients in different countries; Chinese and South Korean patients are more likely to utilize CAM for IBD than are Japanese patients (Table 4). Despite uncertainty, this difference might be attributed to the unique health care system of traditional oriental medicine, which mainly accounts for the CAM services or products in each country. For instance, China and South Korea have a similar pattern of national policies and resources and a formal educational system of traditional medicine [28]. These 2 countries include traditional medicine in the national health care system and have their own educational course for doctors specializing in traditional medicine, whose position is defined by the law and regulated by the government, probably resulting in a high level of social acceptance of CAM in the general population. In contrast, Japan has no formal system of traditional medicine; only herbal mixtures known as Kampo and some acupuncture are included in the health care system [28]. Furthermore, no official educational system exists specific to traditional medicine in Japan [28]. This might suggest that varied historical and cultural background might explain the disparity of perception among countries. The different accessibility to CAM use in each country would be another reason for the different perception among countries.
Intriguingly, there was a gap in the perception of CAM between South Korean patients with IBD and doctors; South Korean patients favored CAM (Table 4), whereas South Korean doctors were less likely to think CAM was an effective method of addressing IBD (Fig. 2). Although we could not explain this disparity in perceptions between patients and doctors in South Korea, this finding suggests a possible greater risk of poor doctor-patient relationships with respect to CAM use in South Korea. However, a recent study showed that more Korean patients with IBD have negative attitudes toward CAM use regarding its effectiveness compared to a decade ago probably due to reliable information from the internet, advent of social media and activation of on-and-offline IBD communities in the recent years [24].
Apart from the nationality of patients, we identified current active disease as another independent predictor of CAM use, which is consistent with the results of previous study [7]. This finding indicates that sicker patients with IBD are more likely to use CAM.
Of note, relaxation was considered a helpful form of CAM for IBD by most physicians, which is in line with the position statement of the European Crohn’s and Colitis Organization [29]. Several studies have shown that relaxation reduces symptoms and improves quality of life in patients with IBD [30,31]. However, we found that moxibustion/cupping was the most frequently used CAM service by patients, which is not supported by the literature [29]. Furthermore, although probiotics were the most used CAM by patients and were considered a beneficial/recommendable form of CAM by most doctors in our study, growing evidence does not support the role of probiotics in the management of IBD; only specific strains seem to be effective in UC [29]. Hence, adequate education guided by evidence is necessary for IBD patients to use CAM optimally.
We acknowledged the failure to obtain information on education level, socio-economic status such as income, insurance system and adherence to IBD treatment of patients from each country as the main limitation of the study because these variables are known to influence CAM usage [18,23,32]. In addition, different educational background or system of the medical school in each country, which was not assessed in the study, might influence doctors’ perspectives. Different age of doctors might also affect their attitude to CAM use as young and senior physicians may have different levels of exposure to CAM.
In summary, this study demonstrated that the prevalence of CAM use for IBD in East Asian countries does not differ from the prevalence in their Western counterparts (8.6% for CAM services and 29.7% for CAM products). We found that there was a significant gap with respect to CAM usage among different East Asian countries, not only from the patients’ perspective but also from the physicians’ point of view. This disparity might be attributed to the different historical and cultural backgrounds of traditional medicine in each country.
Notes
Funding Source
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest
Park DI is an editorial board member of the journal but was not involve in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Author Contribution
Study concept, design, analysis of data: Kim ES. Study concept, design: Ogata H. Substantial contribution to the acquisition and interpretation of data for the work: Tae CH, Jung SA, Park DI, Im JP, Eun CS, Yoon H, Jang BI, Fukuhara K, Hirai F, Ohtsuka K, Liu J, Cao Q. Drafting of the manuscript: Kim ES. Critical revision of the manuscript: Ogata H. Approval of final manuscript: all authors.
Supplementary Material
Supplementary materials are available at the Intestinal Research website (https://www.irjournal.org).
Supplementary Table 1. Prevalence of CAM Use According to Different Indications Among Patients with IBD from 3 Countries
ir-2020-00150-suppl1.pdfSupplementary Table 2. Characteristics of Physicians from 3 Countries
ir-2020-00150-suppl2.pdfSupplementary Material. Questionnaire
ir-2020-00150-suppl3.pdf