A striking flail chest: a rare manifestation of intestinal disease
Article information
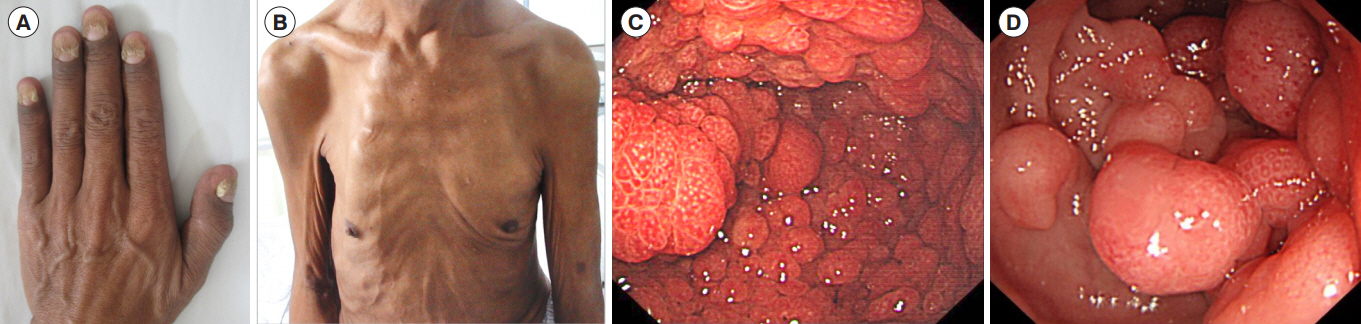
Question: A 59-year-old male patient was admitted to the department of gastroenterology for intermittent diarrhea for 4 years, anorexia and weight loss. He had hyperpigmentation of skin (Fig. A) and oral mucosa, alopecia and nail dystrophy (Fig. A). He had no family history of colon cancer or GI polyps. A flail chest (bilateral chest wall collapse) (Fig. B) and paradoxical breathing were noticed on physical examination. Laboratory tests showed severe deficiency of 25 hydroxyvitamin D (7.4 μg/L), elevated parathyroid hormone (92 pg/mL), normal serum calcium and alkaline phosphatase. The chest CT scan revealed bilateral, multiple rib fractures (right rib, 2–11; left rib, 2–11). A gastroduodenoscopy and a colonoscopy revealed hundreds of polymorphic polyps lining the stomach (Fig. C), duodenum and the whole colon (Fig. D). Histopathology of this patient showed hyperplastic polyps in antrum and colon and villoustublar adenoma in colon (Informed consent to publish was taken from the patient). What is the diagnosis of this patient?
Answer to the Images: Cronkhite-Canada Syndrome
A clinic-pathologic diagnosis of Cronkhite-Canada syndrome (CCS) was made based on the above findings.
CCS is a rare, non-hereditary disease characterized by widespread GI polyposis and ectodermal abnormalities [1]. The diagnosis of CCS should be based on characteristic clinical, endoscopic, radiologic and histologic findings [2]. GI symptoms and ectodermal abnormalities were prominent in this patient. Endoscopy showed typically CCS polyps that distributed among the entire GI tract except oesophagus [3]. It is necessary to differentiate CCS from other GI polyposis syndromes such as Peutz-Jeghers syndrome, juvenile polyposis syndrome, Gardner syndrome and Turcot syndrome when polyposis of GI tract is noted under endoscopy [4]. The diagnosis of CCS is usually delayed due to low incidence and unrecognized phenotype. Although not considered as a malignant disorder, the mortality of CCS is high, mainly due to complications such as GI bleeding, malabsorption and rectal prolapse [2]. In this case, the patient suffered from severe osteoporosis and osteomalacia due to the deficiency of vitamin D. To the best of our knowledge, flail chest caused by CCS has not been described in the literature up to now.
Considering the high mortality of CCS due to diverse complications, it is important to achieve early diagnosis and appropriate treatment. Thus, we suggest gastroenterologists be cognizant of the typical manifestations and diagnostic methods to better identify CCS. Gastroenterologists should also be aware of the potential danger of CCS-related osteoporosis and osteomalacia for better disease management.
Notes
FINANCIAL SUPPORT
This work was supported by specialized scientific research fund project for healthcare industry (201002020) and Teaching Quality Project of Peking Union Medical College (2017zlgc0110).
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION
Conceptualization: Liu S and Li J. Methodology: formal analysis: funding acquisition: Qian JM and Li J. Project administration: Qian JM. Visualization: You Y. Writing-original draft: Liu S. Writing-review and editing: Ruan GC, You Y, and Li J. Approval of final manuscript: all authors.