The elderly population are more vulnerable for the management of colorectal cancer during the COVID-19 pandemic: a nationwide, population-based study
Article information
Abstract
Background/Aims
The impact of coronavirus disease 2019 (COVID-19) on the management of colorectal cancer (CRC) may worse in elderly population, as almost all COVID-19 deaths occurred in the elderly patients. This study aimed to evaluate the impact of COVID-19 on CRC management in the elderly population.
Methods
The numbers of patients who underwent colonoscopy, who visited hospitals or operated for CRC in 2020 and 2021 (COVID-19 era) were compared with those in 2019, according to 3 age groups (≥70 years, 50–69 years, and ≤49 years), based on the nationwide, population-based database (2019–2021) in South Korea.
Results
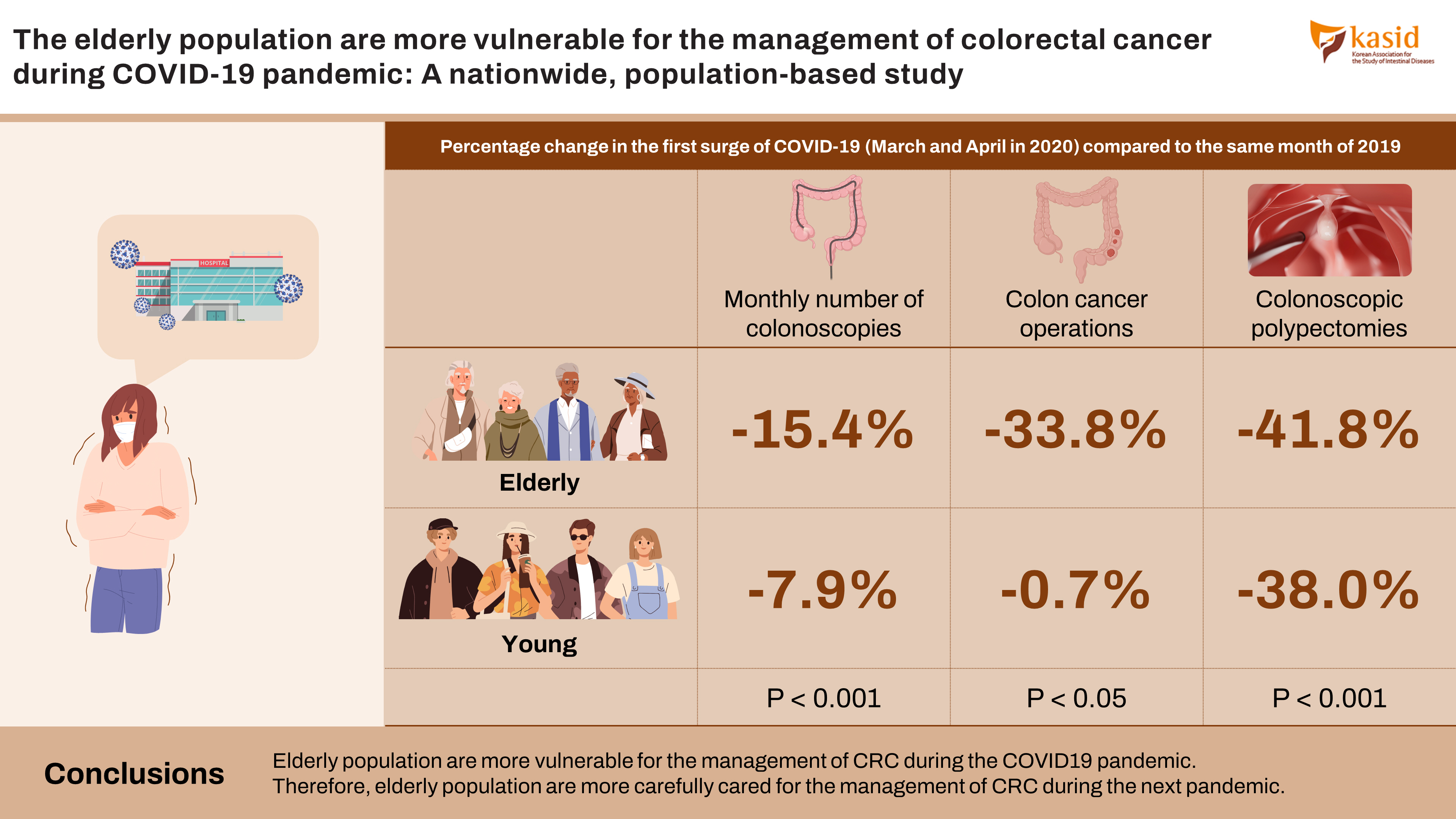
The annual volumes of colonoscopy and hospital visits for CRC in 2020 were more significantly declined in the old age group than in the young age group (both P<0.001). In addition, the annual volume of patients operated for CRC numerically more declined in old age group than in young age group. During the first surge of COVID-19 (March and April 2020), old age patients showed statistically significant declines for the monthly number of colonoscopies (–46.5% vs. –39.3%, P<0.001), hospital visits (–15.4% vs. –7.9%, P<0.001), CRC operations (–33.8% vs. –0.7%, P<0.05), and colonoscopic polypectomies (–41.8% vs. –38.0%, P<0.001) than young age patients, compared with those of same months in 2019.
Conclusions
Elderly population are more vulnerable for the management of CRC during the COVID-19 pandemic. Therefore, the elderly population are more carefully cared for in the management of CRC during the next pandemic.
INTRODUCTION
In South Korea, the first case of novel coronavirus disease 2019 (COVID-19) was reported on January 20, 2020 [1]. After the declaration of the COVID-19 pandemic by the World Health Organization on March 12, 2020, several outbreaks of the COVID-19 occurred in South Korea between 2020 and 2021. The American Gastroenterological Association recommended that all elective procedures, such as screening and surveillance colonoscopy, should be delayed in asymptomatic patients during the COVID-19 pandemic [2]. The Korean Cancer Association guidelines also recommended that colorectal cancer (CRC) screening should be determined according to the shortage of medical resources and the COVID-19 status of the region [3]. Therefore, the COVID-19 pandemic has declined the number of screening and management of CRC in the world [4,5].
The impact of COVID-19 on the screening and management of CRC may worse in elderly population than in younger population, as almost all COVID-19 deaths occurred in elderly patients [6,7]. In a systematic review and meta-analysis of 42 studies with 423,117 patients, elderly patients had increased mortality due to COVID-19 with a pooled odds ratio of 2.6, and a hazard ratio of 1.3 [6]. In other systematic review and meta-analysis of 59 studies, elderly patients ( ≥ 70 years) had a higher infection risk with a relative risk (RR) of 1.7, a higher risk for severe COVID-19 disease with a RR of 2.1, an increased need for intensive care with a RR of 2.7, and a higher mortality with a RR of 3.6, compared with patients younger than 70 years [7]. Currently, no population-based studies have quantified the negative effect of COVID-19 on the management of CRC in the elderly population. A better understanding of the impact of the COVID-19 pandemic on colonoscopy and CRC management in the elderly population may be the first step toward the successful rearrangement of medical resources for the elderly population.
This study aimed to evaluate the impact of the COVID-19 pandemic on colonoscopy and CRC management in the elderly population.
METHODS
1. Data Source
This was a nationwide population-based study using the Health Insurance Review and Assessment (HIRA) database of South Korea. In South Korea, the National Health Insurance (NHI) program covers approximately 98% of the total population with universal health coverage [8,9]. All healthcare providers and all Koreans are required to be covered under the NHI program, which is based on fee-for-services [9]. HIRA data is generated in the process of reimbursing providers under the NHI and contains comprehensive information on the relevant healthcare services, including various procedures, operations, examinations, treatments, and prescriptions [9]. Procedure codes in physician claims databases had a very high level of agreement with data in medical charts. The index date for extracting the study data from the HIRA database was August 1, 2022.
2. Study Population
In this study, the COVID-19 era was defined as the period from January 1, 2020 to December 31, 2021, as the first case of COVID-19 was reported in January 2020 and several outbreaks had continued to December 2021. In South Korea, the first surge of COVID-19 was encountered at March and April 2020 with the implementation of social distancing. During the COVID-19 era, the Korean government offered guidance on changes in standard medical practices to minimize COVID-19 transmission. As a result, many Koreans postponed colonoscopy to avoid exposure to COVID-19 [2], and CRC patients also delayed their hospital visit and operations for the CRC during the COVID-19 era.
We compared the claims of colonoscopy, hospital visit for CRC, and operations for CRC during the COVID-19 era (2020–2021) and pre-COVID-19 era (2019) as a reference. In this study, 3 age groups were defined as follows: young age ( ≤ 49 years), middle age (50–69 years), and old age ( ≥ 70 years) population. The young and middle age cutoff was based on the official age (50 years) for CRC screening in guidelines [10]. The middle age and old age cutoff were based on a systematic review and meta-analysis, which reported that patients aged ≥ 70 years had a higher rate of COVID-19 infection, severe COVID-19 disease, an increased need for intensive care, and higher mortality compared with patients younger than 70 years [7]. As the information used in this study was related only to pseudonyms, the requirement for informed consent was waived. This study was approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong, Seoul, Republic of Korea (IRB number: KHNMC 2022-05-045).
3. Definition of Variables
Data in this study were extracted using the HIRA claim codes [11]. Colonoscopy was defined as colonoscopy without polypectomy (E7660). Colonoscopic polypectomies were defined as a single polypectomy (Q7701), 2 or more polypectomies (Q7702), endoscopic mucosal resection (Q7703), or endoscopic submucosal dissection (QX706). Colonoscopic procedures were analyzed per patient because some patients underwent multiple colonoscopic procedures. CRC was defined as C18 (malignant neoplasm of the colon), C19 (malignant neoplasm of the rectosigmoid junction), C20 (malignant neoplasm of the rectum), and carcinoma in situ of the colon and rectum (D010, D011, and D012) based on the major diagnostic codes of the International Classification of Diseases, ninth revision codes. CRC claim codes in South Korea are reliable, as they are strictly registered in the HIRA system because CRC patients pay only 5% of their medical costs for 5 years by co-payment policy. CRC operations were defined as colectomy (QA671, QA672, QA673, QA679, Q2671, Q2672, Q2673, Q2679, Q1261, or Q1262) and/ or surgical resection of the rectum/sigmoid colon (QA921, QA922, QA923, QA924, Q2921, Q2922, Q2923, Q2924, Q2927, Q9292, QA928, or Q2928) in patients with CRC (Supplementary Table 1).
4. Statistical Analysis
The data during the COVID-19 era (2020–2021) were compared with the results of the same periods in 2019 for monthly and annual comparisons. For the monthly comparison, monthly data of 2019 were compared with those in 2020 and 2021. Descriptive analysis was performed on the entire population during the study period. Annual or monthly comparative analysis between 2 groups were done using the chi-square tests. All statistical tests were two-sided, and a P-value of < 0.05 was considered statistically significant. All statistical analyses were conducted using the R software package (R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org).
RESULTS
1. Claim Data of Colonoscopy
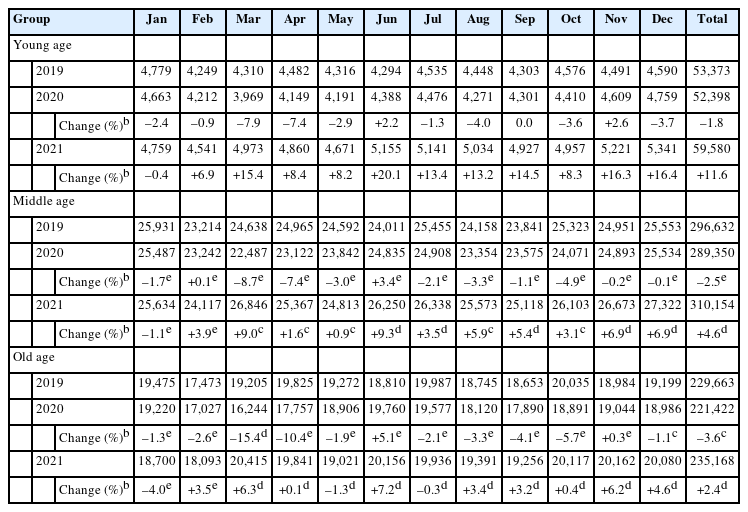
The annual volumes of colonoscopies decreased by 8.7%, 7.0%, and 2.6% in the young age, middle age, and old age groups, respectively, in 2020 compared with those in 2019 (Table 1). The annual volumes of colonoscopies in 2020 significantly declined in middle and old age groups than those in young age group (both P<0.001). However, the annual volumes of colonoscopies in 2021 increased in all age groups compared with those in 2019. During the first surge of COVID-19 (March–April 2020), the monthly number of colonoscopies decreased in all age groups compared with those in 2019, however, they declined more significantly in middle and old age groups than those in young age group (all P<0.05) (Fig. 1). After the first surge of COVID-19 in 2020, the monthly number of colonoscopies slowly recovered in all age groups compared with those in 2019 (Fig. 2).

The monthly change (%) of colonoscopy, hospital visit for colorectal cancer (CRC) and operation for CRC during the first surge of coronavirus disease 2019 (March and April of 2020), compared with those in 2019, more significantly declined in middle and old age groups than young age group (reference). Their statistical significance was expressed with aP<0.05, bP<0.001.

The percentage change of colonoscopy claim in 2020 and 2021, compared to those of 2019, were more significantly declined in middle and old age groups than those in young age group in the first epidemic wave, but slowly recovered in all age groups even in the 2nd-4th epidemic waves. Statistical significance was expressed with aP<0.05, bP<0.001.
2. Claim Data of Hospital Visit for CRC
The annual volume of hospital visit for CRC decreased by 1.8%, 2.5%, and 3.6% in the young age, middle age, and old age groups, respectively, in 2020 compared with those in 2019 (Table 2). The annual volumes of hospital visit for CRC significantly declined in 2020 in old age group than those in young age group (P<0.05). In 2021, the annual volume of hospital visit for CRC was significantly less recovered in old age group than young age group (2.4% vs. 11.6%, P<0.05), compared with those in 2019. During the first surge of COVID-19, the monthly number of hospital visit for CRC were more significantly declined in old age group than young age group (–15.4% vs. –7.9%, P<0.001 in March) (Fig. 1). After the first surge of COVID-19 in 2020, the monthly number of hospital visits slowly recovered in all age groups compared with those in 2019 (Fig. 3).

The percentage change of hospital visit in 2020 and 2021, compared to those of 2019, were significantly declined in old age group than those in young age group in the first epidemic wave, but slowly recovered in all age groups even in the 2nd-4th epidemic waves. Statistical significance was expressed with aP<0.05, bP<0.001.
3. Claim Data of Operation for CRC
The annual volume of patients operated for CRC decreased by 0.8%, 3.5%, and 5.8% in the young age, middle age, and old age groups, respectively, in 2020 compared with those in 2019 (Table 3). The annual volume of patients operated for CRC numerically more declined in old age groups than those in young age group, however, did not reach statistical significance. The annual volumes of patients operated for CRC in 2021 increased in all age groups compared with those in 2019. During the first surge of COVID-19, the monthly number of patients operated for CRC in 2020 decreased in all age groups, compared with those in 2019. However, they declined more significantly in old age group than those in young age group (–33.8% vs. –0.7%, P<0.05 in April) (Fig. 1). After the first surge of COVID-19 in 2020, the monthly number of patients operated for CRC slowly recovered in all age groups compared with those in 2019 (Fig. 4).

The percentage change of colorectal cancer (CRC) operation in 2020 and 2021, compared to those of 2019, were significantly declined in old age group than those in young age group in the first epidemic wave, but slowly recovered in all age groups even in the 2nd-4th epidemic waves. Statistical significance was expressed with aP<0.05, bP<0.001.
4. Claim Data of Colonoscopic Polypectomy
The annual volumes of colonoscopic polypectomies increased in all age groups in 2020 and 2021 compared with those in 2019 (Table 4). During the first surge of COVID-19, the monthly number of colonoscopic polypectomies declined in all age groups compared with those in 2019, however, more significantly declined in middle and old age groups than young age group (both P<0.001). After the first surge of COVID-19 in 2020, the monthly number of colonoscopic polypectomies rapidly recovered in all age groups compared with those in 2019.
DISCUSSION
This population-based study quantify the impact of the COVID-19 pandemic on colonoscopy and CRC management in elderly population. The annual volumes of colonoscopy and hospital visits for CRC in 2020 were more significantly declined in old age group than in young age group. In addition, the annual volume of patients operated for CRC numerically more declined in old age group than in young age group. During the first surge of COVID-19 (March–April 2020), elderly subjects showed statistically significant declines for the monthly number of colonoscopies, hospital visits, CRC operations, and colonoscopic polypectomies than young age patients, compared with those in same month of 2019. Our study results were consistent with those of Western studies [12,13], in that the annual volume of colonoscopy and CRC management markedly decreased during the COVID-19. But, our notable finding was that elderly patients are more vulnerable for the management of CRC during the first surge of COVID-19 pandemic. In South Korea, the first surge of COVID-19 in March and April 2020 was followed by 2nd epidemic wave in July to October 2020, 3rd epidemic wave from November 2020 to February 2021 and 4th epidemic wave from July to September 2021 [14]. Despite several epidemic waves of COVID-19, colonoscopy and management of CRC were gradually unaffected by COVID-19 epidemic changes after the first surge of COVID-19 in South Korea.
In recent studies [7,15-17], old age was an independent risk factor for COVID-19 mortality. In a UK-based study, elderly patients aged ≥ 75 years showed a 13-fold higher COVID-19 mortality risk compared with those aged < 65 years [15]. In a systematic review and meta-analysis, individuals aged ≥ 75 years had a 3.4-fold higher risk for COVID-19 mortality [16]. Based on 178,568 COVID-19 deaths from approximately 2.4 billion U.S. population, elderly patients aged ≥ 65 years had significantly higher COVID-19 mortality rates compared with younger individuals [17]. In a recent meta-analysis including 59 studies comprising 36,470 patients, elderly patients aged ≥ 70 years had a higher rate of COVID-19 mortality, COVID-19 infection, severe COVID-19 disease, and need for intensive care compared with patients younger than 70 years [7]. Due to the higher risk of COVID-19 transmission and mortality among elderly patients, the screening and management of CRC may be more decreased in the elderly patients than in young age group during the COVID-19 pandemic.
Therefore, efforts are needed to close the gap of colonoscopy and CRC management in the elderly population during the first surge of COVID-19. The gap of CRC management may be reduced by converting contact treatment to non-contact treatment for the elderly population. In the United States, for example, hospital visits decreased by 68%, but, telemedicine visits increased by 41% during COVID-19 [18]. In addition, colonoscopy may be converted to fecal immunochemical test (FIT) to reduce the backlog of elderly subjects who need to be screened for CRC [19]. FIT is a relatively non-contact and safe procedure, therefore, FIT could be an alternative to colonoscopy to elderly subjects, who are hesitant of hospital visits during COVID-19 [20]. However, colonoscopy is still preferred over FIT due to higher diagnostic yield of CRC. So, stool DNA-based test with a high diagnostic yield for CRC may be promising option for elderly subjects during COVID-19. A recent study showed that stool DNA-based methylated syndecan-2 test has increased sensitivity (90.2%) and specificity (90.2%) for detection of CRC as compared to FIT [21]. This test could be done entirely from home with no special preparation during COVID-19.
Temporary interruption of CRC screening and management during the COVID-19 pandemic may lead to additional deaths from CRC. In Canada, 6-month interruptions in CRC screening due to COVID-19 will lead to increase of CRC incidence until 2200 with more CRC deaths over the lifetime [22]. In the United Kingdom, a 12-month delay of CRC diagnosis due to COVID-19 was estimated to decrease in 6.4% of 5-year survival rate of CRC [18]. In addition, they expected to take 3–6 months for the return to pre-pandemic levels even after lifting all restrictions on CRC screenings [23]. Therefore, a substantial increase in the number of avoidable CRC deaths may be expected as a result of diagnostic delays of CRC during COVID-19. In our study, the volume of colonoscopies declined during only the first surge of COVID-19 (March–May 2020), which may little impact on the oncological outcomes of CRC. However, oncological outcomes of CRC affected by COVID-19 pandemic should be further evaluated in South Korea, especially for the elderly population.
The use of the HIRA database enabled us to perform the first Asian study to date that assessed the worse impact on the elderly population for the colonoscopy and CRC management during COVID-19. Our findings are virtually free from referral bias and are readily generalizable owing to the population-based design. However, this study has some limitations. One of the limitations of our study is the secondary data with uncertainty regarding the accuracy of the diagnosis. However, previous studies using the HIRA database have shown that procedures and diagnoses are accurately coded. No specific details regarding the indications of colonoscopy and detailed clinical information of each patient were recorded in the HIRA. In addition, it is challenging to generalize our findings to other countries, as the COVID-19 status and healthcare systems differ in each country. Finally, our population-based data included only 3 years of data, so they are not timely enough, but most timely available. Furthermore, there is a growing body of evidence to suggest similar findings observed internationally.
In conclusion, elderly population are more vulnerable for the colonoscopy and CRC management during the first surge of COVID-19 pandemic. Therefore, elderly population are more carefully cared for the colonoscopy and CRC management during the next pandemic.
Notes
Funding Source
The work was supported by a grant (21153MFDS601) from Ministry of Food and Drug Safety in 2022.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Data Availability Statement
Not applicable.
Author Contributions
Conceptualization: Cha JM. Data curation: Kang HS, Jeon SH, Park SB. Formal analysis: Kang HS, Yoon JY, Kwak MS. Funding acquisition: Cha JM. Methodology: Yoon JY, Kwak MS, Cha JM. Supervision: Cha JM. Writing - original draft: Kang HS, Cha JM. Writing - review & editing: Cha JM. Approval of final manuscript: all authors.
Supplementary Material
Supplementary materials are available at the Intestinal Research website (https://www.irjournal.org).
Supplementary Table 1.
Operation Codes for Colorectal Cancers