First aid with color atlas for the use of intestinal ultrasound for inflammatory bowel disease in daily clinical practice
Article information
Abstract
Intestinal ultrasound (IUS) is a promising modality for the management of inflammatory bowel disease (IBD) and has the potential to particularly contribute in monitoring disease activity, an advantage crucial for optimizing the therapeutic strategy. While many IBD physicians appreciate and are interested in the use of IUS for IBD, currently only a limited number of facilities can employ this examination in daily clinical practice. A lack of guidance is one of the major barriers to introducing this procedure. Standardized protocols and assessment criteria are needed such that IUS for IBD can be considered a feasible, reliable examination in clinical practice, and multicenter clinical studies can be conducted for further clinical evidence of the application of IUS in IBD for best patient care. In this article, we provide an overview of how to start IUS for IBD and introduce basic procedures. Furthermore, IUS images from our practice are provided as a color atlas for understanding sonographic findings and scoring systems. We anticipate this “first aid” article will be helpful to promote IUS for IBD in daily practice.
INTRODUCTION
The prevalence and incidence of inflammatory bowel disease (IBD) are rapidly increasing worldwide [1]. Clinical outcomes have improved with the advancement in therapeutic options and strategies, including molecular-targeted medications [2,3]. Currently, the “treat-to-target strategy” is widely accepted as a concept for optimizing the IBD treatment to achieve mucosal healing and further goals beyond clinical remission [4]. Thus, monitoring disease activity with appropriate timing, intervals, and tools (e.g., biomarkers and imaging examinations) is a crucial clinical challenge. Endoscopic examination is the gold standard for IBD management. In addition, computed tomography (CT) and magnetic resonance imaging have been widely used. However, for endoscopic examination, bowel preparation is required before the examination of the lower gastrointestinal tract, which can be a burden for patients indicated for endoscopy, particularly a colonoscopy, repeatedly. Moreover, although the risk of endoscopic examination is not considered high, endoscopy-related adverse events should be carefully considered. Previous clinical studies have proved the usefulness of CT and magnetic resonance imaging in assessing IBD activity [5,6]. However, these techniques have several limitations: (1) waiting time for the examination (not real-time examination); (2) fasting or drinking bowel preparation solution before an examination; (3) cost; (4) radiation exposure in CT; and (5) adverse events related to contrast agents (particularly in CT). Hence, there is an unmet clinical need for a noninvasive, inexpensive, rigorous, reproducible, and real-time examination technique to directly and repeatedly assess intestinal inflammation over time. Intestinal ultrasound (IUS) is currently considered a promising procedure to address this gap. With advancements in technology, ultrasound machines that can sufficiently image intestinal lesions are more widely available. In addition, several guidelines and statements mention the usefulness of IUS as a diagnostic and monitoring technique for IBD [6-10]. The advantages of IUS are (1) a real-time examination without the need for special preparation by the patient, (2) repeatability over time, (3) minimal cost, (4) extremely low risk of procedure-related adverse events (even during pregnancy [11]), and (5) the ability to assess both intestinal lesions and extra-bowel complications [12]. Several studies have demonstrated the usefulness of IUS for monitoring the treatment efficacy in IBD [13-15]. Moreover, a recent study suggested that early IUS can predict the response to steroid therapy in hospitalized patients with severe ulcerative colitis (UC) [16]. At this point, in clinical practice, IUS for IBD (IBD-IUS) can be employed particularly for overtime monitoring disease activity including treatment response. Meanwhile, it should be noted that IBD-IUS may not be able to evaluate some bowel segments due to intestinal gas or anatomical features and there is a limitation in assessing mucosal surface in detail only with IBD-IUS. At least for now, IBD-IUS cannot replace endoscopy for the surveillance of UC-associated neoplasia. In the treat-to-target strategy, IBD-IUS cannot directly assess histological healing in UC because not able to obtain biopsy specimens, while IBD-IUS may be more useful to evaluate transmural healing in Crohn’s disease (CD) than endoscopy. Although the combination of IUS and other modalities is required for compensating the limitations of each examination, IUS could reduce the frequency of other burdensome, expensive modalities.
While many IBD physicians now realize that IUS is a promising modality in their daily practice and are interested in performing IUS, one of the major challenges seems to be the lack of a guideline to learn the procedure, including an atlas of sonographic images. The quality of IUS can depend on an examiner, and performing and assessing IUS using standardized procedures is believed to be crucial for reliable evaluation contributing to IBD management. Therefore, although practicing IUS in the clinical setting can be the best method to improve the skills and the fact that some diagnostic criteria remain controversial, we would like to provide this “first aid” approach with a color atlas for using IUS in daily clinical practice for IBD so that more physicians and sonographers feel comfortable with the procedure, and IBD-IUS becomes a more common imaging examination in the clinical setting.
BEFORE INITIATING IUS
1. Machine Setting
First, a sonography machine for IUS should be prepared. In IBD-IUS, observation with B mode and color Doppler is common. With appropriate settings, both a convex probe and a linear probe can be used for IBD-IUS. A convex probe can push intestinal gas away with proper pressure more easily and obtain a wider view of the deep area compared to a linear probe. A linear probe can provide a wider view of the area near the body surface than a convex probe. Although no specific criteria have been established, a probe frequency of approximately 5–10 MHz is considered sufficient for B mode scanning [13,14,17-19]. Meanwhile, a lower-frequency probe (up to around 6 MHz) is useful for screening intestinal complications. It should be noted that the image quality can vary between machines even with the same probe frequency. For color Doppler, the velocity range should be set at approximately 4–7 cm/s [14,19-21]. This value can differ between machines. However, this setting should be ensured to be different from that for the common abdominal examination (e.g., liver, gallbladder, and pancreas), which usually employs >15 cm/s. More parameters should be established to optimize sonographic images, such as gain and contrast; however, evaluators need not be overwhelmed. The machine manufacturer may simply be asked to introduce the intestinal preset. Each manufacturer should have an intestinal preset (a default setting for intestinal examination) suitable for obtaining typical intestinal images with each machine. The preset may be used and arranged based on an individual’s experience and preference.
2. Preparations before IBD-IUS
One of the major advantages of IBD-IUS is that specific preparations by a patient are not necessary, except for some special cases requiring detailed IUS for the upper gastrointestinal tract. A patient can eat and drink before the examination and does not need to take any laxatives. In general, we ask our patients to come for the examination while continuing their daily eating habits so that the “physiological” condition of the intestines can be assessed. We believe this is crucial, particularly for patients with CD because fasting may make the stenotic lesion less apparent. Patients are only asked to avoid urination before IUS if possible to facilitate easier observation of the rectum. However, IUS can still be performed even for patients who have just used the restroom prior to the examination. For transabdominal IUS, the patient should be instructed to roll up the shirt and the pants/skirt down to examine the entire abdominal area (Fig. 1). After instructing the patient to lie on his/her back on the examination table with the appropriate drape, the preparation before IUS is all set.

Examination of the colon using transabdominal ultrasound. We start from the middle lower area to examine the rectum. The rectum cannot be sufficiently assessed with transabdominal ultrasound. Then, we trace the colon counterclockwise. In some cases, the transverse colon descends from the middle to the lower abdominal area.
3. Basic Procedures of IBD-IUS
The primary goal in IBD-IUS is to complete the transabdominal ultrasound. First, the colon should be carefully assessed. We evaluate the colon counterclockwise (Fig. 1). We understand that some examiners prefer performing the examination clockwise. We believe that both approaches are effective as long as the colon is assessed continuously. Some key points should be considered for sufficient and efficient examination. First, distinguishing the colon and the small intestine is crucial. The colon has the haustra structure, and peristalsis is lesser in the colon than in the small intestine (Fig. 2A). In the large and small intestines, 5 layers are typically observed in the wall (Fig. 2B). The normal thickness of the intestinal wall remains controversial; however, our facility employs a threshold of <2 mm in the small intestine [13], <3 mm in the colon [22], and <4 mm in the rectum [20]. Then, recalling the typical anatomic features of the colon is helpful to identify segments of the colon: (1) the ascending colon and descending colon are fixed on the retroperitoneum; (2) the sigmoid colon crosses the iliopsoas muscle and iliac artery and vein at the left lower quadrant; and (3) the rectum is located dorsal to the bladder and prostate or vagina. In point (1), the ascending colon and descending colon should be at “the most lateral” and “the most dorsal” sides of the trunk. Observation from the lateral or dorsal side can be helpful. Point (2) is a crucial landmark to identify the sigmoid colon (Fig. 3). Once the crossing part is found, the sigmoid colon can be traced to the oral and anal sides for detailed observation. Although assessing the rectum via transabdominal IUS is generally challenging, considering point (3), we do our best to observe the rectum. As per our experience, a part of the rectosigmoid can be observed even in patients with undetected upper rectum and lower rectum. Transperineal ultrasound can be an option for patients requiring assessment of the anorectal area [20,23,24], and the procedure is further described later in this article.
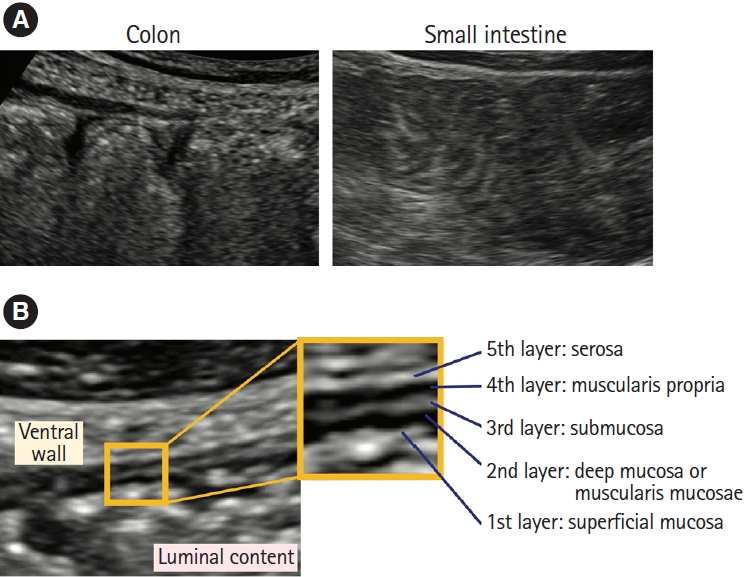
Sonographic images of the normal large and small bowel. (A) The overall B-mode image of the colon and small intestine. The colon exhibits the haustra, whereas the Kerckring’s fold is observed in the small intestine. During an examination, distinguishing the difference in peristalsis (lesser in the large bowel than in the small bowel) is also helpful. (B) The bowel has a 5-layer wall stratification: The 1st layer (hyperechoic) is the surface of the mucosa (superficial mucosa); 2nd layer (hypoechoic), the mucosa (deep mucosa) or muscularis mucosae; 3rd layer (hyperechoic), the submucosa; 4th layer (hypoechoic), the muscularis propria; and 5th layer (hyperechoic), the serosa.
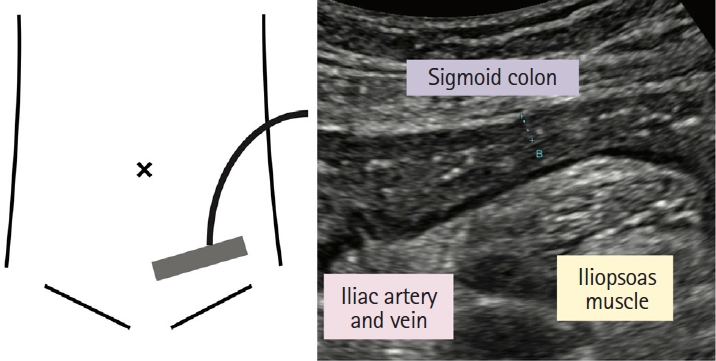
The landmark for identifying the sigmoid colon. At the left lower quadrant, the iliopsoas muscle and iliac blood vessels can be landmarks in identifying the sigmoid colon. The image is that of a patient with ulcerative colitis.
After examining the colon, the small intestine is assessed next. Because we examine the colon counterclockwise, the ileocecal valve is identified as the last step. Once the ileocecal valve is identified, the terminal ileum should be traced to the oral side to evaluate the distal ileum. Generally, the terminal ileum is observed at the right lower quadrant, and its oral side appears to cross the iliopsoas muscle and iliac blood vessels and then disappears to the right pelvic cavity (Fig. 4A). To screen small intestinal lesions and complications, particularly in CD, the sonography probe is moved as shown in Fig. 4B. We believe a probe with up to ~6 MHz (the so-called low–middle frequency) is better than ~10 MHz (the so-called high frequency) for the screening, although no strict evidence/recommendation has been established to date. In cases when abnormal peristalsis, dilation, or looping of the intestine or hyperechoic mesenteric fat are found during the screening procedure, these findings suggest the presence of intestinal lesions and/or complications, and the specific area should be examined in detail, considering the change in probe frequency. After the transabdominal ultrasound, transperineal ultrasound can be performed for further assessment of the rectum and perianal area, particularly for CD.
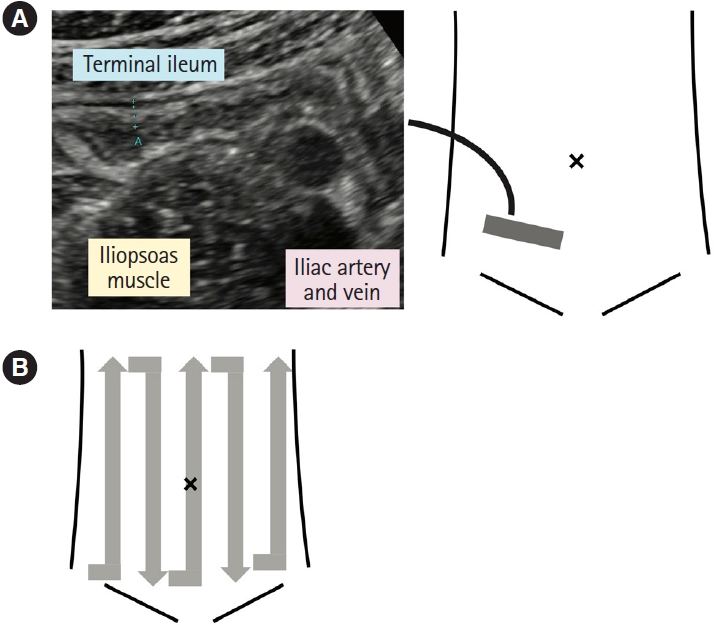
Examination of the small intestine. (A) Ileocecal valve is identified while observing the ascending colon and cecum and then the terminal ileum can be followed from the ileocecal valve. At the right lower quadrant, the iliopsoas muscle and iliac blood vessels can be landmarks in identifying the sigmoid colon. This image is that of a patient with Crohn’s disease. (B) We screen the small bowel in the entire abdomen by moving the sonographic probe.
4. Major Sonographic Parameters for IBD Assessment
At present, IUS parameters, including (a) bowel wall thickness (BWT), (b) bowel wall flow (BWF), (c) bowel wall stratification (BWS), (d) haustration of the colon, (e) mesenteric fat echogenicity (inflammation of fat, i-fat), and (f) peri-intestinal lymph nodes (LNs), are widely used to assess IBD disease activity [19,25]. In addition to these parameters, given that the thickened submucosa is one of the typical sonographic findings in UC, we previously reported the usefulness of the ratio of submucosal thickness to total BWT to estimate the endoscopic severity [21]. The interobserver reliability of BWT (mm) has been reported to be almost perfect (intraclass coefficient, 0.96; 95% confidence interval [CI], 0.92–0.98) and that of BWF (presence/absence of increased Doppler signal) exhibited almost perfect agreement (κ=0.83, 95% CI, 074–0.92) in IUS for UC [19]. BWT also showed almost perfect agreement in patients with CD (intraclass coefficient, 0.96; 95% CI, 0.94–0.98) [25]. Several scoring systems have been developed, such as the Milan Ultrasound Criteria [18,26] and UC-IUS index [27] for UC and the Simple Ultrasound Score for CD [17] and International Bowel Ultrasound Segmental Activity Score (IBUS-SAS) [25] for CD, using some of the abovementioned parameters. We would like to highlight that understanding key images of each sonographic parameter, including the normal condition, and interpreting sonographic findings in a standardized manner are necessary so that IUS can be a reliable, reproducible examination method. We prepared a color atlas of major sonographic parameters (a) to (f) described above for a colleague in our facility. Here, we would like to share the atlas and other representative sonographic images, anticipating that they will be of some help to improve our examination quality and consistency and, eventually, contribute to better patient care in the IBD field.
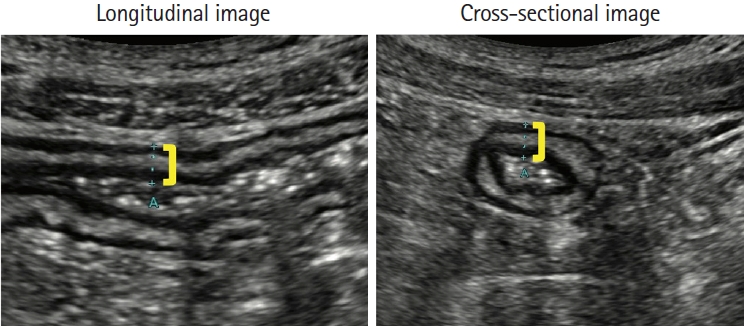
1) Bowel Wall Thickness
For each segment of the intestine, we measure BWT at the most severely affected part (i.e., the part with the most thickened wall) longitudinally and cross-sectionally. The key point is measuring BWT vertically to the intestinal wall (Fig. 5). As mentioned above, our threshold for the normal BWT is <2 mm in the small intestine and <3 mm in the colon. Measuring the wall thickness of the rectum precisely with transabdominal ultrasound is challenging, although we employ the normal threshold of the rectum of <4 mm.
2) Bowel Wall Flow
BWF is generally assessed with color Doppler. It is crucial to use the appropriate setting of the color Doppler for the intestine and realize the limitation that the too-deep area (e.g., >5 cm from the probe) cannot be sufficiently evaluated. A patient may need to hold breathing during the color Doppler examination. Limberg score (LS) [28] is widely used. This scoring system considers both wall thickness and vascularity. As the original LS employs a threshold of 4 mm for the normal BWT, 3 mm for the colon and 2 mm for the small intestine were considered. Therefore, we strictly use the modified LS (Fig. 6). Meanwhile, the IBUS-SAS [25] scoring system focuses on vascularity. Therefore, LS of 0 and 1 are IBUS-SAS of 0, and LS of 2, 3, and 4 are IBUS-SAS of 1, 2, and 3, respectively (Fig. 6).
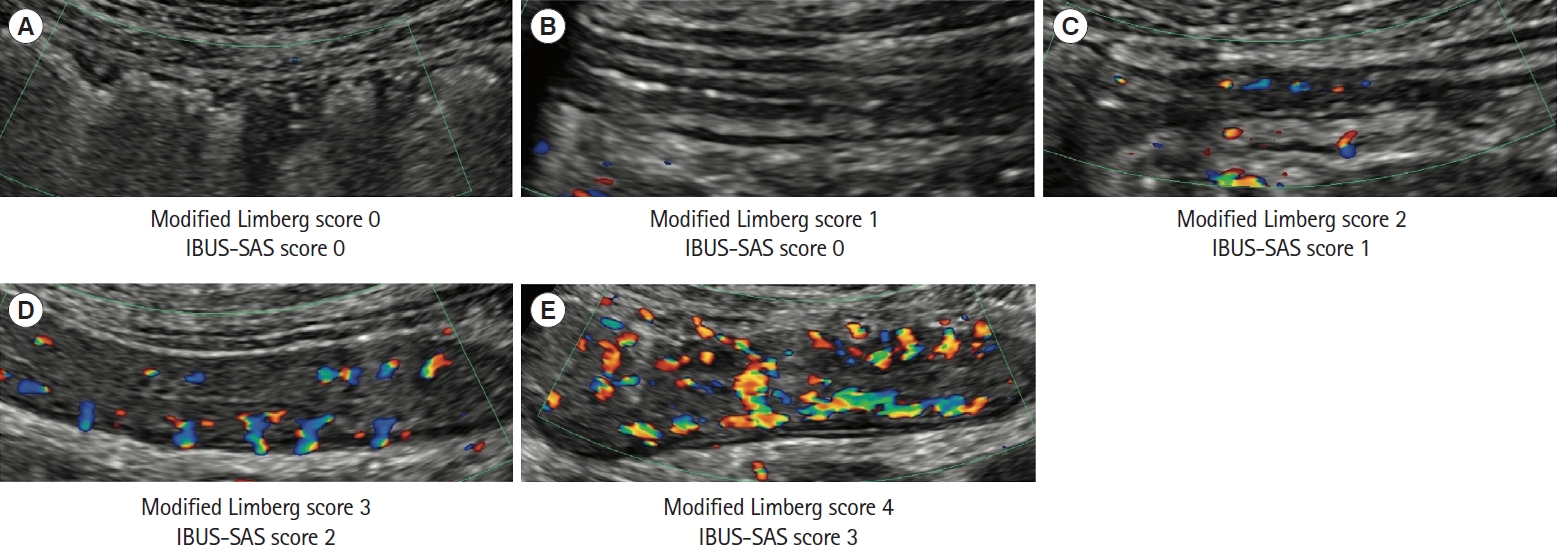
Bowel wall flow. The bowel wall flow is generally assessed using color Doppler. The machine setting is crucial for appropriate examination. (A) Normal bowel wall thickness without color Doppler signal. (B) Thickened bowel wall without color Doppler signal. (C) Point-like, short color Doppler signals. (D) Linear-appearance color Doppler signals. (E) Long color Doppler signals extending the bowel wall and the surrounding mesenteric tissue. The velocity range of color Doppler for these images was 4.2 cm/s. IBUS-SAS, International Bowel Ultrasound Segmental Activity Score.
3) Bowel Wall Stratification
The assessment of BWS can be described as normal stratification, uncertain stratification, and loss of stratification (LOS). In normal stratification, 5 layers can be observed. The key point is particularly the clear identification of the hyperechoic third layer. We consider stratification to be uncertain when the third layer is visible but the borders of the layer are vague. In LOS, the layers in the wall cannot be identified, i.e., the hyperechoic third layer cannot be distinguished from the hypoechoic fourth layer (Fig. 7). We evaluate BWS as normal, uncertain, and loss in our facility. The IBUS-SAS [25] scores normal stratification as 0, uncertain stratification as 1, LOS with a length of ≤3 cm as 2, and LOS with a length >3 cm as 3, although the threshold significance of 3 cm in LOS may need further discussion.
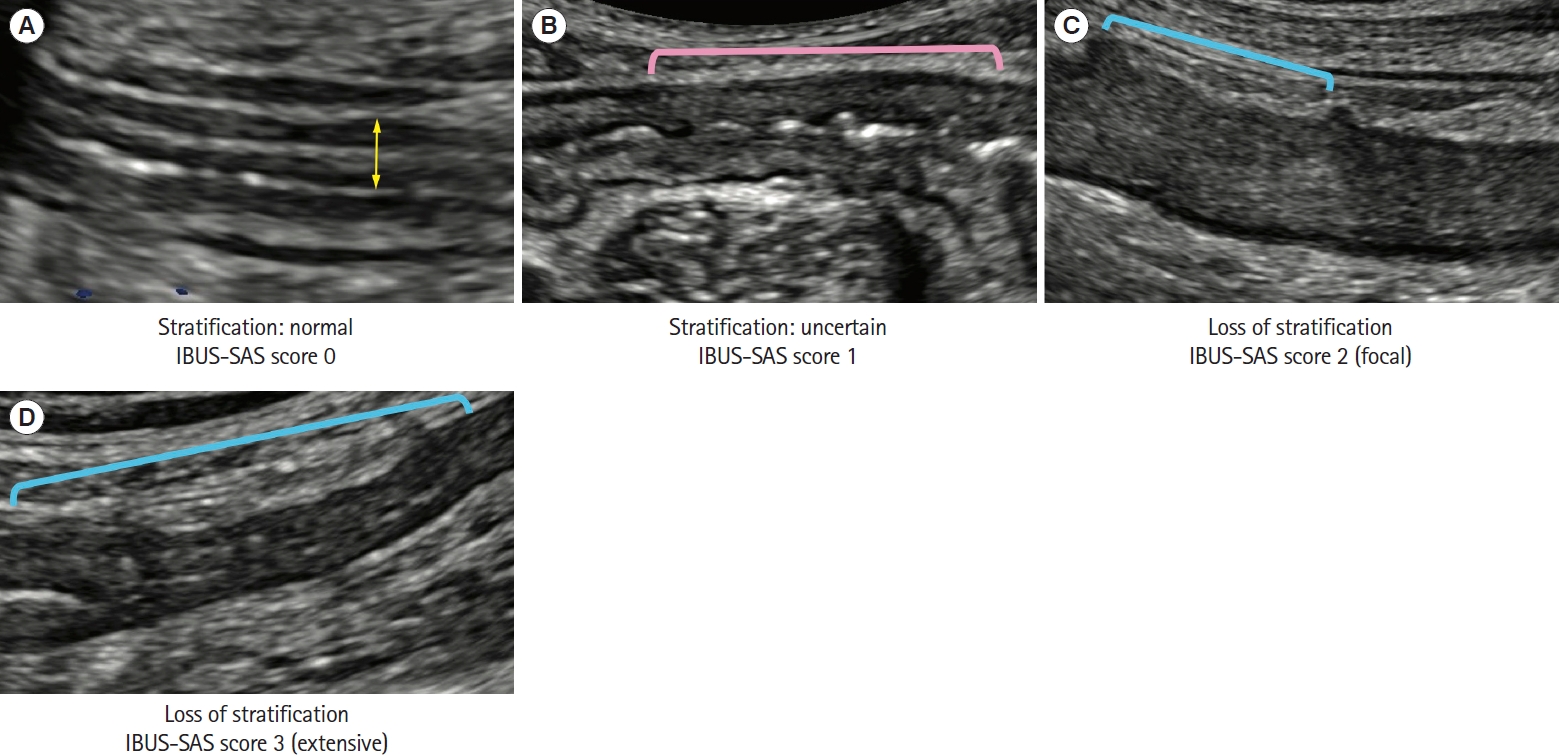
Bowel wall stratification. (A) The normal 5-layer stratification. The yellow line represents bowel wall thickness. (B) The pink line indicates the area with uncertain bowel wall stratification. (C) The blue line indicates the area with loss of stratification. This image represents a focal loss of stratification (≤3 cm). (D) The blue line indicates the area with loss of stratification. This image represents an extensive loss of stratification (>3 cm). IBUS-SAS, International Bowel Ultrasound Segmental Activity Score.
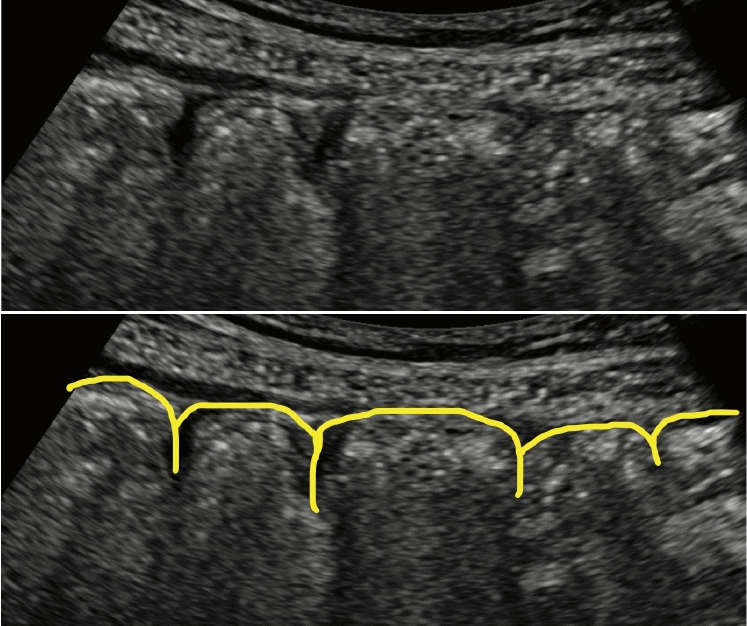
4) Haustration of the Colon
The normal colon has a haustration structure (Fig. 8). The inflamed segments of the colon may lose this structure (Fig. 7). We evaluate this parameter as preserved or lost in our facility. When the haustration structure in a colon segment is observed to be lost, we record the segment as lost. A study on UC, which employed a scoring system of 0 for preserved, 1 for uncertain (in doubt of complete loss of haustrations), and 2 for loss, showed a fair interobserver agreement (κ=0.24; 95% CI, 0.13–0.35) [19].
5) Mesenteric Proliferation (Inflammation of Mesenteric Fat [i-fat])
In each intestinal segment, we assess the presence or absence of hyperechogenicity of the mesenteric fat surrounding the segment compared with the overall echogenicity of the mesenteric fat (Fig. 9). This finding suggests i-fat. In case of severe i-fat, the whole mesenteric fat shows hyperechogenicity, and the contrast between the mesenteric fat (high) and intestine (low) is prominent, a finding we call the isolation sign (Fig. 7C and D). This is one of the reasons why a severely inflamed intestine is easily detected. The IBUS-SAS scores were 0, 1, and 2 for the absence, uncertainty, and presence of i-fat, respectively. The interobserver agreement for i-fat detection was moderate in CD (κ=0.51; 95% CI, 0.34–0.67) [25], whereas a study on UC showed a fair agreement (κ=0.36; 95% CI, 0.17–0.55) [19].
6) Peri-intestinal LNs
Swollen LNs can be observed around the intestine in some patients, particularly in young patients with severe inflammation (Fig. 10). Although we employ the threshold of 5 mm in the shortest axis as a swollen LN following a previous report [19], it still seems controversial, and we record the maximum length of the shortest axis of LNs in our daily practice.
5. Other Sonographic Findings in IBD-IUS
1) Thickened Submucosa
In UC, even in patients with maintained BWS, the submucosa (the third layer) appears thickened (Fig. 11), a typical finding in UC, which can also be observed in CD.
2) Ulcer
When there is a deep ulcer, the border between the luminal content and the intestinal wall appears to exist inside the wall and is observed as a hyperechogenic spot or line (Fig. 12). In the case of many broad deep ulcers, the wall-stratification layers are lost, and the intestinal wall appears thin, suggesting a high-risk situation (Fig. 12B).

Ulcer. (A) Both panels are identical sonographic images. The bottoms of the ulcers are observed inside the wall (yellow arrowheads). The orange line indicates the luminal surface. (B) The bowel wall appears thin due to the loss of wall tissues in the area with broad deep ulcers (blue line). The yellow arrowheads indicate ulcers.
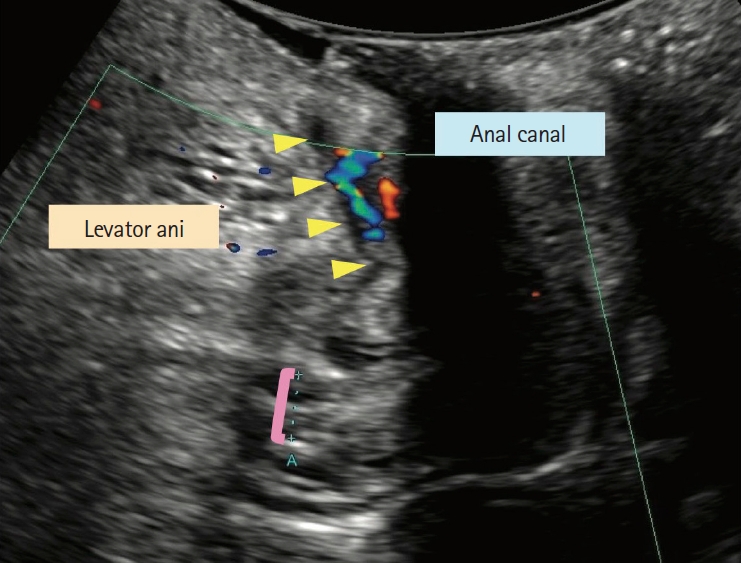
3) Transperineal Sonography for Anorectal Area
Although transabdominal ultrasound is the mainstream application of IBD-IUS, it has a limitation in assessing anorectal area. Transperineal ultrasound can potentially provide information on this area [20,23,24].Generally, the patient is asked to wear examination underwear for a colonoscopy and lies on his/her left side while bending knees, similar to the procedure during a colonoscopy. Subsequently, the examiner gently presses the probe against the patient’s anus (no need to insert), and longitudinal images of the anorectal area are observed (Fig. 13). The key step is sufficiently pushing down the probe. Although the procedure is not physically invasive, the examiner should carefully consider the patient’s privacy and emotional stress. In transperineal ultrasound, we assess the same sonographic parameters as in transabdominal ultrasound.
4) Intestinal Complications
IBD, particularly CD, can cause various intestinal complications. IUS is useful for assessing those complications [12]. The fistula is generally detected as a hypoechoic narrow luminal structure (diameter, <2 cm) [29], and the gas and/or liquid flow can be observed (Fig. 14A and B). The abscess is typically hypoechoic but can show various echogenicities and small hyperechoic particles can be observed inside. Notably, vascularity is increased in the surroundings of the abscess without vascularity inside the abscess (Fig. 14C and D). In some countries and regions, contrast-enhanced US is approved for diagnosing abscesses in IBD-IUS, and, if available, this pr ocedure provides additional clinical information. Stenosis and bowel obstruction in the small intestine are also common CD complications. At the stenotic lesion with bowel obstruction, we observe dilation (>3 cm) [30] and/or abnormal acceleration of peristalsis of the oral-side small intestine (Fig. 14E). Interestingly, some stenotic lesions demonstrate increased vascularity, whereas others do not. We speculate that the difference reflects inflammatory versus fibrotic stenosis.
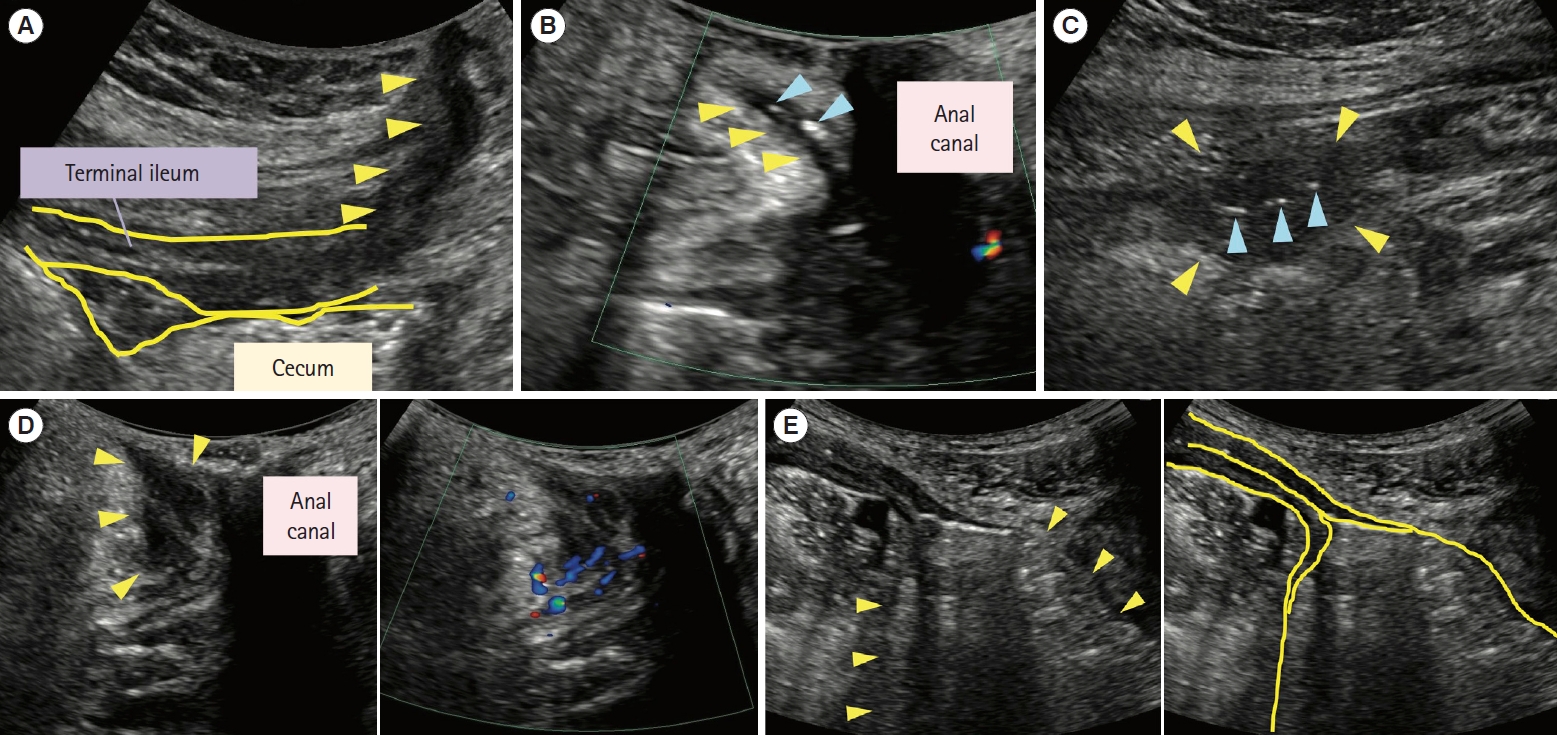
Intestinal complications observed using ultrasound examinations. (A) The fistula between the terminal ileum and skin is shown (yellow arrowheads). An adhesion can be observed between the terminal ileum and cecum. (B) This perineal ultrasound image shows a perianal fistula (yellow arrowheads). The hyperechoic objects compatible with gas are observed in the fistula (blue arrowheads). (C) The hypoechoic area surrounded by yellow arrowheads is an abscess. Some hyperechoic objects compatible with gas (blue arrowheads) are observed inside the abscess. (D) This perianal ultrasound image shows a perianal abscess (surrounded by yellow arrowheads). Color Doppler signals are detected around the abscess. (E) Both panels are identical sonographic images. The dilation of the ileum (yellow arrowheads) occurs due to terminal ileum stenosis. The velocity range of color Doppler for images (B) and (D) was 4.2 cm/s.
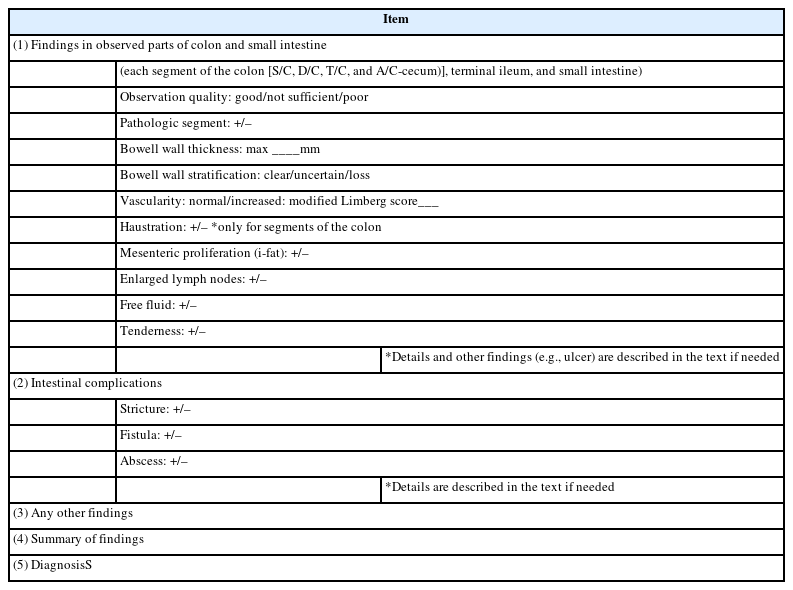
6. IBD-IUS Reporting System
A comprehensive report is a crucial component of the examination. Moreover, we believe the key is adequate communication among examiners and IBD physicians such that the IUS can contribute to clinical decision-making, especially in the current situation wherein not all IBD physicians are familiar with IUS. Therefore, each facility should consider the reporting format/system. We recommend the report should mention the major sonographic parameters and findings, interpretations, and diagnosis. Changes from a previous examination constitute crucial information. Some illustrations can help understand the examination results, particularly in a complicated case wherein describing the findings in the text is challenging. Table 1 and Fig. 15 demonstrate examples of electronic text reports in our medical record system and hand-drawn reports (scanned to the medical record system eventually), respectively.

Hand-drawn report format in our facility. (A) Each format is used mainly for ulcerative colitis and Crohn’s disease. (B) An example illustration of the ileocecal area extracted from a hand-drawn report. In this patient with Crohn’s disease, inflammation is observed in the oral side of the ascending colon and the cecum, and these parts appear distorted with inflammatory fat and the local collection of ascites. With distortion, the ileocecal valve is observed at the ventral side of the cecum, and adhesion is detected between the terminal ileum and ventral side of the cecum (yellow arrowheads). The ileum is also inflamed, showing loss of stratification with mesenteric proliferation.
FUTURE PERSPECTIVES
While several IBD-IUS scoring systems have been developed to estimate endoscopic activity [17,18,25-27], determining whether sonographic findings and scores can be associated with the prognosis of patients with IBD is crucially challenging. In this context, “sonographic remission” should be defined, particularly for transmural healing in CD. Moreover, although the main inflammatory site of UC has been thought to be mucosa, IUS suggests that it also has transmural changes. The significance of this finding and its impact on UC management remains unestablished. Addressing these challenges will provide insights for optimizing IUS in the treat-to-target strategy.
CONCLUSION
IBD-IUS is not a unique technique. Once the basic points are understood, this noninvasive examination can be applied in daily practice. We hope that this article will be helpful for physicians and sonographers as the first step of IBD-IUS. In addition, we highlight that with the rapidly increasing evidence of IUS in the IBD field and more advanced technologies (e.g., microvascular imaging and elastography), the knowledge and skills of operators should be continuously updated.
Notes
Funding Source
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest
Miyoshi J received consultation and lecture fees from AbbVie GK, EA Pharma Co., Ltd., Janssen Pharmaceutical K.K., and Takeda Pharmaceutical Co., Ltd. Morikubo H received a grant from Takeda Pharmaceutical Co., Ltd. Hisamatsu T received consultation and lecture fees from Mitsubishi Tanabe Pharma Corporation, AbbVie GK, EA Pharma Co., Ltd., Kyorin Pharmaceutical Co., Ltd., JIMRO Co., Ltd., Janssen Pharmaceutical K.K., Mochida Pharmaceutical Co., Ltd., and Takeda Pharmaceutical Co., Ltd.; and received research grants from Alfresa Pharma Co., Ltd., EA Pharma Co., Ltd., Mitsubishi Tanabe Pharma Corporation, AbbVie GK, JIMRO Co., Ltd., Zeria Pharmaceutical Co., Ltd., Daiichi-Sankyo, Kyorin Pharmaceutical Co., Ltd., Nippon Kayaku Co., Ltd., Takeda Pharmaceutical Co., Ltd., Pfizer Inc., and Mochida Pharmaceutical Co., Ltd. Except for that, no potential conflict of interest relevant to this article was reported.
Data Availability Statement
Not applicable.
Author Contributions
Supervision: Hisamatsu T. Writing - original draft: Miyoshi J, Morikubo H, Yonezawa H, Mori H. Writing - review & editing: Miyoshi J, Morikubo H, Yonezawa H, Mori H, Hisamatsu T. Approval of final manuscript: all authors.