How the COVID-19 pandemic affected the severity and clinical presentation of diverticulitis
Article information
Abstract
Background/Aims
Single-institution studies showed that patients presented with more severe diverticulitis and underwent more emergency operations during the coronavirus disease 2019 (COVID-19) pandemic. Therefore, we studied this trend using nationwide data from the American College of Surgeons National Surgical Quality Improvement Program database.
Methods
Patients (n = 23,383) who underwent a colectomy for diverticulitis in 2018 (control year) and 2020 (pandemic year) were selected. We compared these groups for differences in disease severity, comorbidities, perioperative factors, and complications.
Results
During the pandemic, colonic operations for diverticulitis decreased by 13.14%, but the rates of emergency operations (17.31% vs. 20.04%, P < 0.001) and cases with a known abscess/perforation (50.11% vs. 54.55%, P < 0.001) increased. Likewise, the prevalence of comorbidities, such as congestive heart failure, acute renal failure, systemic inflammatory response syndrome, and septic shock, were higher during the pandemic (P < 0.05). During this same period, significantly more patients were classified under American Society of Anesthesiologists classes 3, 4, and 5, suggesting their preoperative health states were more severe and life-threatening. Correspondingly, the average operation time was longer (P < 0.001) and complications, such as organ space surgical site infection, wound disruption, pneumonia, acute renal failure, septic shock, and myocardial infarction, increased (P < 0.05) during the pandemic.
Conclusions
During the pandemic, surgical volume decreased, but the clinical presentation of diverticulitis became more severe. Due to resource reallocation and possibly patient fear of seeking medical attention, diverticulitis was likely underdiagnosed, and cases that would have been elective became emergent. This underscores the importance of monitoring patients at risk for diverticulitis and intervening when criteria for surgery are met.
INTRODUCTION
On March 11, 2020, the World Health Organization declared the coronavirus disease 2019 (COVID-19) a pandemic [1]. During this time, hospitals became overwhelmed with high volumes of COVID-19 patients and were subsequently tasked to reallocate medical resources to manage and treat COVID-19 [2,3]. This increased peoples’ reluctance to present to the emergency department for acute illnesses out of fear of nosocomial infections [4-8] and even changed the paradigm of how surgical ailments, such as diverticulitis, were managed. Across the country non-emergent or elective operations for these patients were canceled or postponed [3,9], and nonoperative and outpatient methods to manage diverticulitis were employed [3,10]. However, whether it was due to changes in resource reallocation, patients’ reluctance to present to the emergency department, or even abdominal manifestations of COVID-19 itself [11], single-institution studies have begun to show how the clinical presentation and severity of diverticulitis have profoundly worsened during the pandemic. For example, Hossain et al. [12] demonstrated that the absolute number of acute diverticulitis cases decreased by 51% at their hospital, but the number of emergency operations and cases classified as Hinchey II, III, or IV increased significantly. Zintsmaster and Myers [8] reported that the incidence of abscesses among patients with diverticulitis more than doubled during the pandemic (11.70% vs. 4.40%, P < 0.01). To this date, thirteen case studies have reported that COVID-19 may have severe extrapulmonary manifestations, such as gastrointestinal involvement [11]. Altogether, these findings are novel to the medical literature and underscore changes in the clinical presentation and severity of diverticulitis during the pandemic at single institutions. To our knowledge, there are no publications using nationwide data regarding these observations. This prompted us to analyze national data from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) to study this trend.
METHODS
The primary goal of our analysis was to shed light on how the volume, clinical presentation, and severity of diverticulitis have changed during the pandemic. We studied these changes by comparing the rates of emergency operations, cases involving perforation and/or abscess, comorbidities, and differences in American Society of Anesthesiologists (ASA) classification among patients presenting with diverticulitis prior to and during the pandemic. Additionally, we analyzed differences in morbidity and mortality to ascertain whether there were significant changes in patients’ clinical outcomes. The following complications were included in our analyses: superficial incisional surgical site infection (SSI), deep incisional SSI, organ/ space SSI, wound disruption, pneumonia, unplanned intubation, pulmonary embolism, on ventilator > 48 hours, progressive renal insufficiency, acute renal failure, urinary tract infection, stroke, cardiac arrest requiring cardiopulmonary resuscitation, myocardial infarction, transfusion, deep vein thrombosis requiring therapy, sepsis, septic shock, return to the operating room, hospital stay > 30 days, Clostridium difficile infection, unplanned readmission, and mortality.
For statistical analyses, we utilized chi-square tests to analyze categorical variables, and we used Student t-tests to analyze continuous parameters. These analyses were conducted using Minitab 17.
1. IRB/IACUC Approval
We conducted this study in compliance with the principles of the Declaration of Helsinki. The study’s protocol was reviewed and approved by the Institutional Review Board of Atlantic Health System (IRB No. 1847883-1). This study is a retrospective study using medical record review and so informed consent was waived.
2. Description of Participants
We identified 23,383 patients in the ACS NSQIP database who underwent a colectomy for diverticulitis either in 2018 or 2020. The 2018 population represented the pre-pandemic population and the 2020 population represented the pandemic population. Patients with a postoperative diagnosis of diverticulitis were identified using the variable “PODIAGTX10,” which denotes “Post-op Diagnosis Text” in the Participant Use Data File user guide. Among these patients, only patients who underwent a colectomy were included. We identified these patients using the following Current Procedure Terminology codes: 44139, 44140, 44141, 44142, 44143, 44144, 44145, 44146, 44147, 44150, 44155, 44156, 44157, 44158, 44160, 44204, 44205, 44206, 44207, 44208, 44210, 44211, 44212, 44213, 44661.
All terms used in this paper specific to gender, race, and ethnicity were adopted from the terms outlined and defined in the ACS NSQIP Participant Use Data File User Guide.
RESULTS
1. Demographic Factors
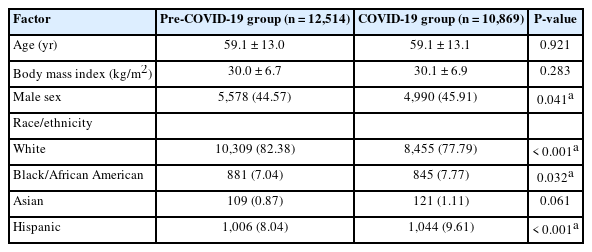
Overall, 23,383 patients who underwent a colonic resection for diverticulitis in either 2018 or 2020 met our inclusion criteria. Between these 2 years, there was an absolute decrease in operative volume for diverticulitis by 13.14% (12,514 cases vs. 10,869 cases). In 2020, otherwise referred to as the pandemic, significant demographic changes were observed. The proportion of Black/African American (7.04% vs. 7.77%, P= 0.032) and Hispanic patients (8.04% vs. 9.61%, P < 0.001) increased. However, there were no significant differences in gender or age (Table 1).
2. Preoperative Comorbidities
Amongst the COVID-19 pandemic population there was a larger proportion of patients seen with significant comorbid conditions. There was a greater incidence of bleeding disorders, > 10% loss in body weight over the past 6 months, wound infection, acute renal failure, and congestive heart failure (P < 0.05) (Table 2).
Additionally, the COVID-19 pandemic population had significantly higher rates of preoperative systemic inflammatory response syndrome (SIRS) and septic shock. The rate of SIRS increased from 2.55% to 3.60% (P < 0.001), and the rate of septic shock increased from 1.77% to 2.35% (P= 0.002) (Table 2).
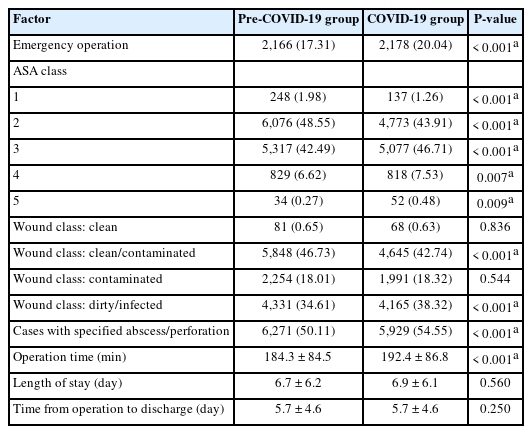
3. Perioperative Factors
The rate of emergency operations (17.31% vs. 20.04%, P < 0.001) and the number of cases with a known abscess or perforation (50.11% vs. 54.55%, P < 0.001) significantly increased among the COVID-19 pandemic population. Additionally, significantly more patients were classified under ASA classes 1 and 2 in the control population, while significantly more patients were classified under ASA classes 3, 4, and 5 in the pandemic population. The rate of ASA classes 4 and 5 increased from 6.62% and 0.27% to 7.53% and 0.48%, respectively (P < 0.05) (Table 3). The rate of operative wounds classified as dirty/infected also increased from 34.61% to 38.32% during the pandemic (P < 0.001) (Table 3). Additionally, the mean operation time was significantly longer for patients during the pandemic. Operation time increased from 184.3 ± 84.5 minutes to 192.4 ± 86.8 minutes (P < 0.001). Of note, no differences in the average length of stay and time from hospital to discharge time were noted (P> 0.05) (Table 3).
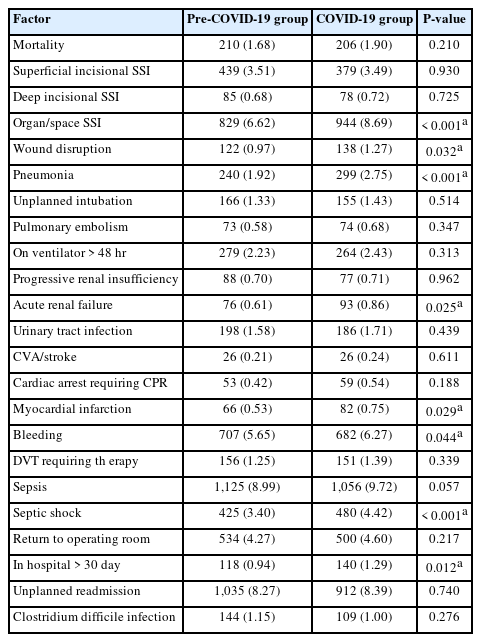
4. Complications and Mortality
Patients developed significantly more postoperative complications during the pandemic, such as acute renal failure, organ space SSI, wound disruption, pneumonia, myocardial infarction, septic shock, and hospital stays > 30 days (all P < 0.05) (Table 4). Organ space SSI increased from 6.62% to 8.69% (P < 0.001), and septic shock increased from 3.40% to 4.42% (P < 0.001). Interestingly, however, there was no difference in mortality (Table 4).
DISCUSSION
Overall, our findings show an absolute decrease in operative volume related to diverticulitis, yet an increase in emergency operations, cases involving an abscess and/or perforation, and rates of SIRS and septic shock during the pandemic. Many single-institution studies showed similar findings [3,7,8,12-14] and have attributed this to a myriad of factors. Cirocchi et al. [9] suggested that general operative volume decreased due to the employment of more conservative medical treatments for diverticulitis in lieu of inpatient or operative management, such as oral antibiotics and percutaneous drainage. Surgical interventions were primarily reserved for patients presenting with symptomology consistent with sepsis or septic shock. This alone contributed to a higher proportion of emergency operations during the pandemic. Furthermore, it is possible that the change in treatments and delay of surgical intervention may allow for their condition to progress and become more severe [2,3,15]. Should conservative measures not be successful, this could lead to more progressive disease and more emergency operations. Costanzi et al. [15] reported a case of perforated diverticulitis, in which the patient initially received nonoperative medical treatment but later underwent an emergency open Hartmann’s procedure due to a dramatic increase in the intrabdominal fluid-gas collection. Additionally, patient hesitation to receive medical care due to fear of contracting COVID-19 can also delay treatment and lead to more progressive disease.
Furthermore, our findings can also be attributed to COVID-19 having extrapulmonary manifestations. For example, several studies showed that COVID-19 enters digestive cells through ACE-2 receptors and can cause a myriad of responses, such as inflammation and gut microbial dysbiosis [16,17]. Case reports have even reported that COVID-19 can exacerbate underlying gastrointestinal ailments, leading to complications, such as bowel perforation [11,17]. Al Argan et al. [11] reported 2 cases in which a patient with a cecal mass and a second patient with diverticulosis both presented with a perforated bowel and concurrent COVID-19 infection. Patel et al. [18] reported a patient who subsequently presented with perforated diverticulitis only 3 days after being discharged for respiratory symptoms from COVID-19. Additionally, Fabbri et al. [19] described a patient who was nonoperatively treated for gastrointestinal symptoms attributed to COVID-19 only to be readmitted for the same symptomology and undergo an urgent operation for perforated sigmoid diverticulitis. At our institution, we have even observed patients who, while paralyzed from mechanical ventilation in the intensive care unit due to COVID-19, also had a concurrent diagnosis of diverticulitis. Many of these patients subsequently developed more severe manifestations without the classic presentation on physical examination [20], which contributes to the high volume of complicated and more severe cases observed nationally during the pandemic.
Intraoperatively, we observed that patients during the pandemic were associated with prolonged operations. It is likely that more open procedures, as opposed to minimally invasive operations, were conducted due to the high rates of emergency operations and severely sick patients during this time [9], which can indirectly contribute to longer operation times.
Patients with diverticulitis during the pandemic developed more complications, such as acute renal failure, organ space SSI, wound disruption, pneumonia, myocardial infarction, septic shock, and hospital stays > 30 days. These patients presented with more comorbidities and had more severe manifestations of diverticulitis at the time of hospital admission, making them more vulnerable to adverse clinical outcomes after surgery. Not only this, but studies suggest that concurrent COVID-19 may be associated with more postoperative complications [21]. Some sources even found that postoperative pulmonary complications occurred in about 50% of patients with a perioperative COVID-19 infection [9,22,23].
Generally, the number of patients whose postoperative recovery lasted less than 30 days did not increase significantly when compared with pre-COVID-19 data. For such stays less than 30 days in each category, antibiotics, intensive care unit care, and cardiovascular and pulmonary support could effectively manage postoperative symptoms, which did not lead to a significant increase in length of stay. Additionally, it is important to recognize the influence of a patient’s status upon admission and that patients with shorter recovery times were likely less ill overall. However, during the COVID-19 pandemic, more severe postoperative complications due to delayed treatment of diverticulitis contributed to longer lengths of stays. This led to a significant increase in the number of patients needing hospital care for more than 30 days during the COVID-19 era.
This study is the first national database study in the United States that shows how the operative volume, clinical presentation, and severity of diverticulitis have changed during the pandemic. However, there are some limitations because of its retrospective design. Fixed datapoints were supplied by the ACS NSQIP, which limited our ability to analyze parameters, such as Hinchey classification, whether patients tested positive for COVID-19 at hospital admission, and date of admission. With admission dates, our analyses could have been centered around studying the first wave of the pandemic when hospital restrictions were enacted. Furthermore, we only show trends for surgery. Therefore, we could not study the severity of diverticulitis among patients who presented to hospitals and underwent non-surgical management.
In conclusion, our analysis of the ACS NSQIP database demonstrates that surgical volume for diverticulitis decreased during the pandemic, yet patients presented with more severe clinical manifestations of diverticulitis. Correspondingly, the rates of emergency surgical intervention and postoperative complications were increased during the COVID-19 time period. There are several possible contributing factors, which include the underdiagnosis of diverticulitis, cancelation of non-emergent or elective operations, employment of nonoperative management of diverticulitis, gastrointestinal manifestations of COVID-19, and delayed presentation of patients due to the fear of contracting COVID-19 at healthcare facilities. Regardless of these reasons, our findings underscore the importance of continuously monitoring patients at risk for diverticulitis and providing surgical intervention when criteria for surgery are met.
Notes
Funding Source
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Data Availability Statement
Not applicable.
Author Contributions
Conceptualization: Rolandelli RH, Soliman SS, Nemeth ZH. Data curation: Soliman SS, Nemeth ZH. Formal analysis: Soliman SS. Investigation: Nemeth ZH. Methodology: Soliman SS, Rolandelli RH, Nemeth ZH. Project administration: Soliman SS, Rolandelli RH, Nemeth ZH. Supervision: Rolandelli RH, Nemeth ZH. Validation: Rolandelli RH, Nemeth ZH. Visualization: Soliman SS, Nemeth ZH. Writing - original draft: Soliman SS, Rolandelli RH, Nemeth ZH, Chang GC, Nemecz AK. Writing - review & editing: Soliman SS, Rolandelli RH, Nemeth ZH, Chang GC, Nemecz AK. Approval of final manuscript: all authors.