|
 |
- Search
| Intest Res > Volume 20(2); 2022 > Article |
|
Abstract
Background/Aims
Methods
Results
ADDITIONAL INFORMATION
Funding Source
This study was supported by a grant (2010-0774) from the Asan Institute for Life Sciences, Seoul, Korea.
Conflict of Interest
Ye BD has received a research grant from Celltrion and Pfizer Korea; consulting fees from Abbvie Korea, Celltrion, Chong Kun Dang Pharm., Daewoong Pharma., Ferring Korea, Janssen Korea, Kangstem Biotech, Korea United Pharm., Medtronic Korea, Shire Korea, Takeda Korea, IQVIA, and Takeda; speaking fees from Abbvie Korea, Celltrion, Ferring Korea, Janssen Korea, Pfizer Korea, Shire Korea, Takeda Korea, and IQVIA. However, the research grant, consulting fees, and speaking fees are not related to the topic of the current study. Yang SK has received a research grant from Janssen Korea, but the research grant was not related to the topic of the current study. The remaining authors have no competing interests to declare.
Myung SJ is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Author Contribution
Conceptualization: Lee SH, Ye BD. Methodology: all authors. Formal analysis: Lee SH, Ye BD. Funding acquisition: Ye BD. Project administration: Ye BD. Visualization: Lee SH, Ye BD. Writing - original draft: Lee SH. Writing - review and editing: all authors. Approval of final manuscript: all authors.
Non-Author Contribution
We thank Bo Sun Kim (Department of Gastroenterology and Inflammatory Bowel Disease Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea) for the laboratory work and Dr. Deepti Chopra (Mount Sinai Hospital, Toronto, Canada) for the language editing of the manuscript.
Supplementary Material
Fig. 1.
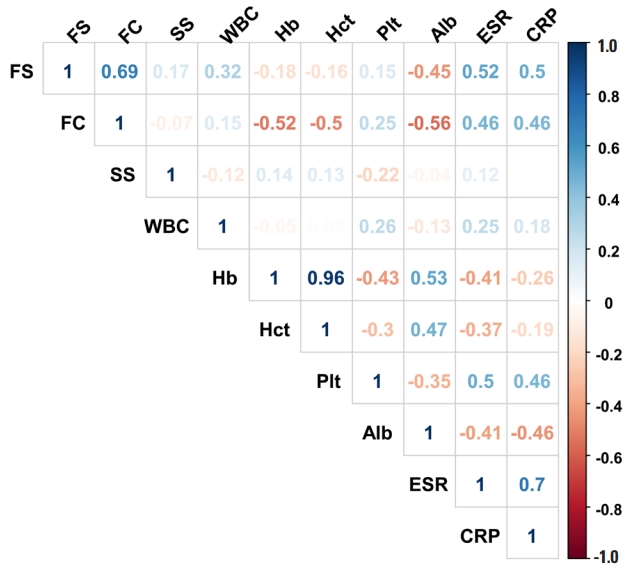
Fig. 2.
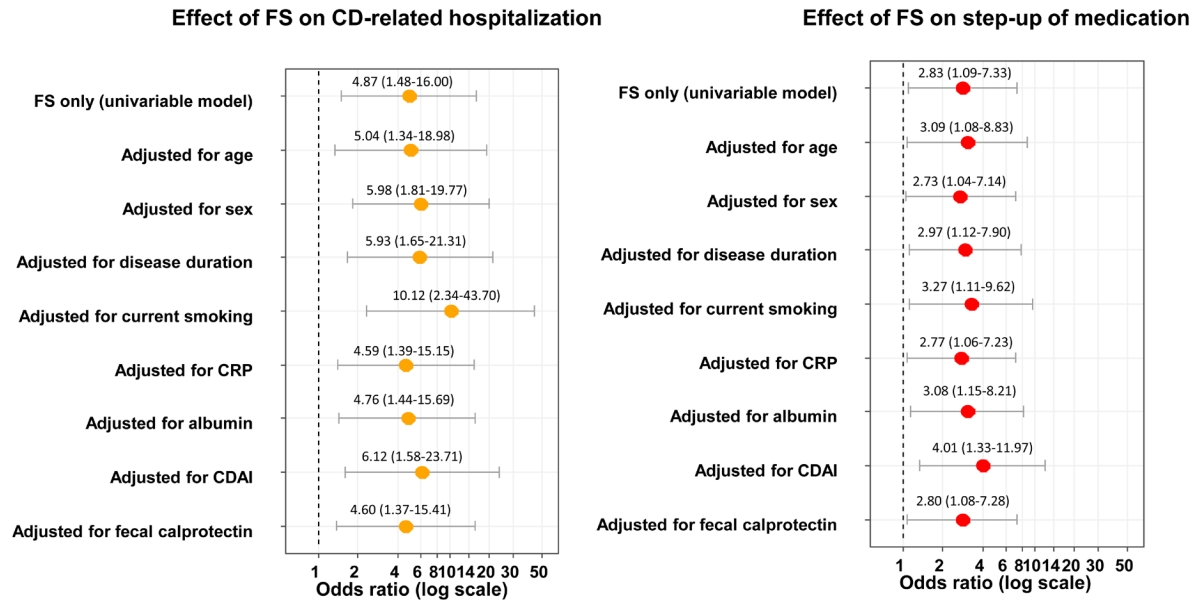
Fig. 3.
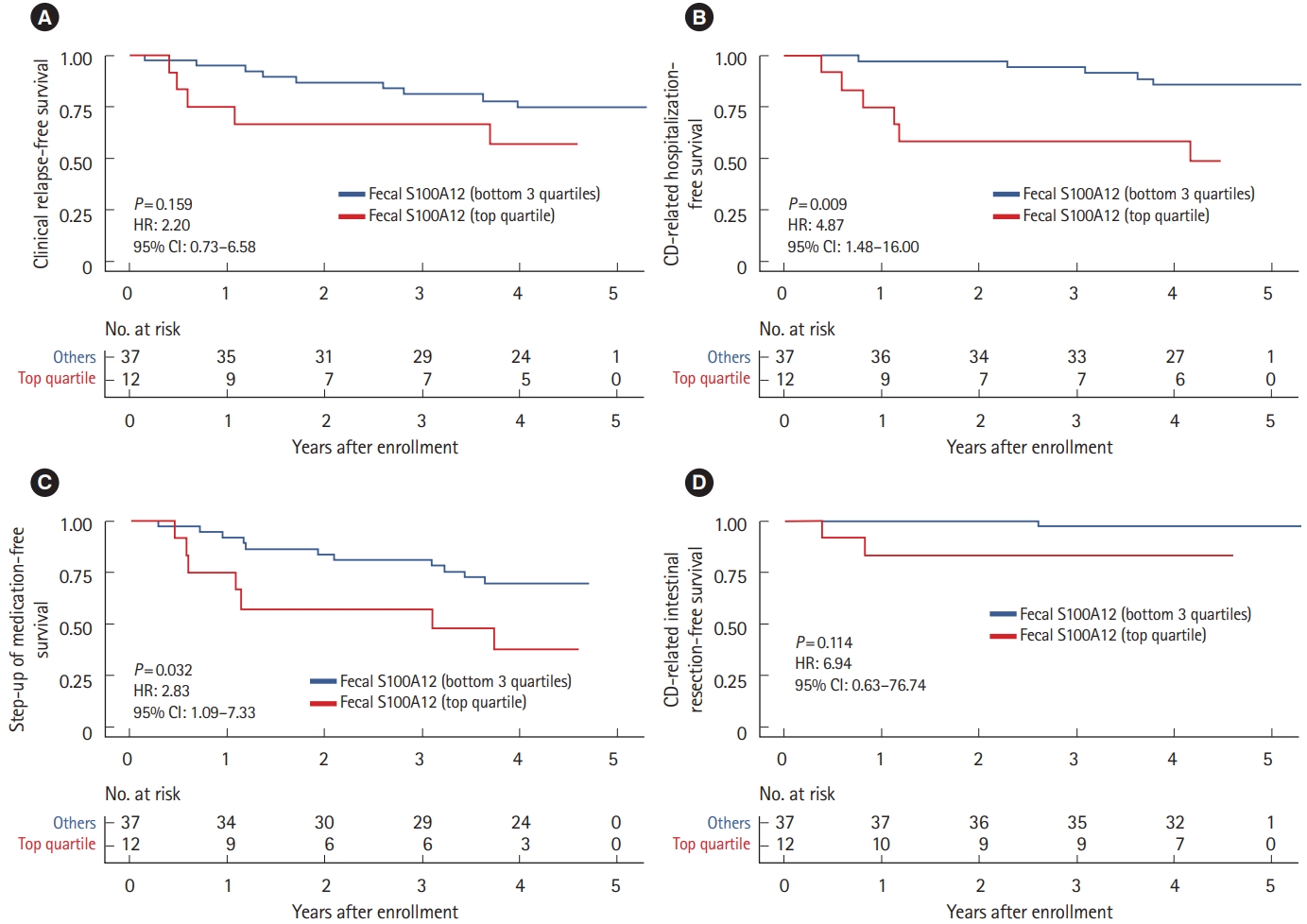
Fig. 4.

Table 1.
Table 2.
| Outcomes | Baseline S100 proteins |
Top quartile vs. othersa |
|||
|---|---|---|---|---|---|
| HR | 95% CI | P-value | c-index | ||
| Clinical relapse | Fecal S100A12 | 2.20 | 0.73-6.58 | 0.159 | 0.591 |
| Fecal calprotectin | 2.58 | 0.89-7.45 | 0.079 | 0.607 | |
| Serum S100A12 | 1.54 | 0.51-4.58 | 0.443 | 0.541 | |
| CD-related hospitalization | Fecal S100A12 | 4.87 | 1.48-16.00 | 0.009 | 0.687 |
| Fecal calprotectin | 1.64 | 0.48-5.59 | 0.432 | 0.555 | |
| Serum S100A12 | 0.55 | 0.12-2.54 | 0.442 | 0.560 | |
| Step-up of medication | Fecal S100A12 | 2.83 | 1.09-7.33 | 0.032 | 0.612 |
| Fecal calprotectin | 1.12 | 0.40-3.15 | 0.826 | 0.512 | |
| Serum S100A12 | 1.45 | 0.54-3.86 | 0.460 | 0.541 | |
| CD-related intestinal resection | Fecal S100A12 | 6.94 | 0.63-76.74 | 0.114 | 0.734 |
| Fecal calprotectin | 5.70 | 0.52-62.86 | 0.156 | 0.701 | |
| Serum S100A12 | 1.37 | 0.12-15.09 | 0.798 | 0.536 | |
Table 3.
| Outcomes (dichotomized variable based on optimal cutoff value) | HR | 95% CI | P-value | c-index |
|---|---|---|---|---|
| Clinical relapse (FS ≥ 0.0136 mg/kg) | 1.35 | 0.42-4.32 | 0.610 | 0.537 |
| CD-related hospitalization (FS ≥ 0.1994 mg/kg) | 6.86 | 2.08-22.60 | 0.002 | 0.711 |
| Step-up of medication (FS ≥ 0.1994 mg/kg) | 4.26 | 1.63-11.10 | 0.003 | 0.638 |
| CD-related intestinal resection (FS ≥ 0.1596 mg/kg)a | 21.64 | 2.09-2,912.40 | 0.008 | 0.885 |